Introduction
In 2013, a Ministerial Advisory Committee on the Prevention and Control of Cancer was instituted1 and tasked with all matters relating to cancer, according to Section 91(1) of the National Health Act. This is documented in the National Cancer Strategic Framework for South Africa 2017-2022.1 This document pertains to all matters relating to malignancies and includes epidemiology, risk factors, current available services and the way forward.
The policy guidelines on the holistic journey of a patient who has a suspected breast malignancy from screening through to palliative care are encompassed in the South African Breast Cancer Prevention and Control Policy (BCPCP) of June 2017.2 This document is aimed at prioritising breast cancer awareness, timely treatment, and adequate palliation for late stage disease.
The 2015 United Nations Sustainable Development Goals form a global blueprint for achieving equality, peace, and prosperity targeted for 2030. Goal 3 (health and wellbeing) speaks directly to healthcare. Other goals, namely 1 (no poverty), 2 (zero hunger), 4 (education), 5 (gender equality), 6 (clean water and sanitation) and 10 (reduced inequality), also play an important role in the access to speedy, quality care. Goal 3.4 reiterates the reduction in the mortality rate of non-communicable diseases by 33%, and Goal 3.8 mandates universal health coverage at affordable rates.3
The Global Cancer Observatory (GCO) (2020) cancer statistics4 revealed that breast cancer (11.7%) is the most common malignancy diagnosed worldwide, with a mortality rate of 6.9%. Cancer-related mortality is reported to be higher in low- to middle-income countries with advanced stages of disease at presentation and delays to treatment. This is reportedly due to lack of awareness and an associated lack of screening and treatment facilities.5
According to South African statistics (2019), breast cancer is recorded as the highest-occurring malignancy in females (23.2%).6 Accurate mortality rates in South Africa are difficult to report on as there is no single governing body following patients for survival. Available figures are based on death certificate information which is inaccurate as it is based on ‘natural’ and ‘unnatural’ deaths only.
Given the paucity of qualified medical oncologists in Gauteng (as well as in South Africa and Africa), waiting times for patients are inevitably expected to be longer than in high-income countries. A report on the global oncology medical burden reported Africa as having some of the busiest oncology practices with a median of over 500 patients seen per institution per year.6,7
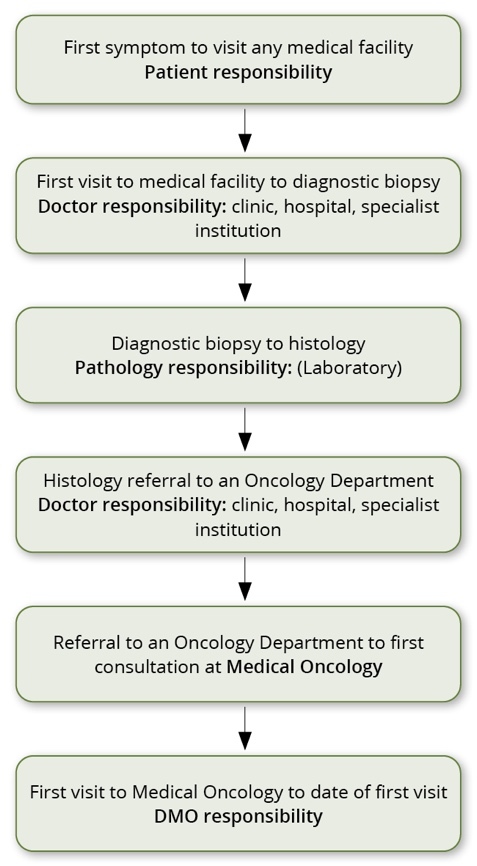
This study was initiated to determine where the longest delays occurred during the patient’s journey, from the first symptom to the first treatment. This information, combined with the existing policy, identifies shortfalls in the breast cancer diagnostic and treatment pathways that must be addressed.
Methods
A cross-sectional, descriptive study design was used to collect data from patients newly diagnosed with breast cancer presenting to the Department of Medical Oncology (DMO), University of Pretoria / Steve Biko Academic Hospital, between August 2020 and April 2021. Patients are seen at the department only if they have been referred from medical institutions and have a confirmed histological diagnosis of breast cancer. Although not planned, this time frame coincided with the COVID-19 pandemic.
The DMO at the University of Pretoria / Steve Biko Academic Hospital, sees patients from Gauteng, Mpumalanga and North West provinces and is estimated to serve a population of more than six million. Steve Biko Academic Hospital is a quaternary public hospital catering mainly to patients requiring specialist and advanced specialist medical care and procedures. Patients presenting to the clinic are mainly from middle- to low socio-economic backgrounds with no medical insurance.
Patients newly diagnosed with breast cancer, who were present in the out-patient department, were approached to take part in the study. Patients who were consulting with the doctor, referred for radiological imaging, or who had already left the department were excluded from the study.
Data were obtained from the patients themselves, with additional clinical data obtained from their medical records. A questionnaire was formulated for the study to collect information on sociodemographic characteristics, patient malignancy knowledge, and clinical data, encompassing the six time points (from first symptom to first treatment) (see Figure 1). The number of visits to medical facilities and dates of staging radiological examinations were also recorded.
Data obtained from the patients about their first symptoms and medical facility visits were recorded in months (no definite date known). In contrast, the remaining periods from the date of the diagnostic biopsy to the date of the first treatment were recorded in days as exact dates for these timelines were recorded. Where months were converted to days, the calculation used was 1 month = 30 days.
Descriptive statistics were used to describe the time from the first symptom(s) to initial treatment and other continuous variables. All analyses were performed using STATA version 15.
Ethics approval was obtained from the Faculty of Health Sciences Research Ethics Committee (#218/2020). Informed consent was obtained from each participant prior to data collection.
Results
During the time frame in question, a total of 220 new patients with breast cancer were booked to be seen in the DMO. Of these, 154 patients arrived for their appointment, 99 of whom were enrolled for the study but 79 were analysed. Reasons for ineligibility included prior treatment (14), existing patients (3), one patient did not have original histology results, one patient presented with a third primary malignancy, and one patient was put on protocol (which would have skewed the data). Table 1 lists the demographic characteristics of the study participants.
Factors which could have had an enabling influence on patient behaviour and corresponding decrease in delay times include family history (prior knowledge of the disease and outcome), transportation (own transport versus relying on public transport), and education level (more exposure to information about the disease). Thirteen patients (16.5%) had a direct family member previously diagnosed with a breast cancer, and ten patients (12.7%) had other relatives with a prior diagnosis of breast cancer. Forty-one patients (51.9%) had their own transport and were not limited to public transport. Most patients (n=57; 72.2%) had secondary education, followed by those with tertiary education (n=14; 17.7%), and primary education (n=4; 6.3%), with only three patients having received no formal education.
Delay information across the six time frames are shown in Table 2. The figures exclude any patients with missing data per time frame.
The longest delays occurred from the first visit to a medical facility to the date of representative biopsy (mean of four months with a range of 0-42 months).
COVID-19 restrictions have not been added for ‘biopsy through referral’ timelines as patient decisions were not necessarily involved in those periods. Most patients (95%) adhered to their initial booked dates for their first visit.
Delays from the first symptom to the first visit to a medical facility
The mean reported patient delays were recorded as three months, ranging from 0-23 months. Reasons for the delay included COVID-19 related restrictions in five patients as well as lack of time, lack of finances (15-month delay), and lack of knowledge of the urgency relating to breast and lymph node changes. Outliers included a patient with a delay of 23 months (reasons not known), 16 months (breast lump would come and go), and 15 months (financial difficulties).
Delays from the first visit to a medical institution to the diagnostic biopsy
There were substantial delays in the time it took medical institutions to perform diagnostic biopsies, with a mean delay of four months in this cohort of patients (range 0-42 months). Eleven patients had a total of 18 non-representative biopsies between them. In five patients who experienced delays of over 12 months, non-representative biopsies, ranging from 1-3, were recorded. These were performed at other institutions and were patient reported. Further information on these biopsies is not available. Repeat biopsies constituted the majority of outlier delay (range 12-42 months). Thirteen patients reported delays due to COVID-19 restrictions during this time.
Of note is that public clinics were the first visit of choice (26 visits), with private general physicians being consulted the second most (25 visits). The balance of the visits included first visits to public hospitals, private hospitals and private specialists (e.g. radiology). Median delay times of participants who first consulted at a public clinic or hospital were seven and four months, respectively, versus 1.5 months for patients who initially consulted at private practices. Twelve patients (15.2%) consulted at one institution before diagnostic biopsy, 39 patients (49.3%) consulted at two institutions before diagnostic biopsy, 18 patients (22.8%) at three institutions, nine patients (11.4%) at four institutions and one patient (1.3%) consulted at five institutions before diagnostic biopsy.
Delays from biopsy to histology
A mean of 16 days (range 0-92 days) was reported from the date of diagnostic biopsy to the final histology. Of the 20 patients with a delay of seven days or less, 11 patients had their tissue diagnosed at a public pathology laboratory, and nine patients utilised a private pathology facility. No reasons for long delays were given.
Delays from histology to referral
The mean delay between histology and referral was 63 days (range 0-894 days). Four patients were referred before the final histology was available. One patient relocated to Limpopo and only returned to seek medical attention after the disease had progressed. Two patients reported having received no further information from the medical institution regarding their results, resulting in the patients querying results and requesting referral.
Delays from referral to the first consultation at Medical Oncology
The mean delay from referral to the first consultation was 25 days (range 0-143 days). Four patients missed their originally booked appointment, and one patient could not attend the clinic due to public transport problems.
Delays from referral to the last radiology test
The mean delay from referral to the last staging radiology test was 21 days (range 0-169 days). Eight patients had their staging radiology done before their first consultation, which enabled early treatment (mean of five days from the first consultation).
Delays from referral to treatment
The mean time from referral to treatment was 18 days (range 0-68 days). Of the patients experiencing long delays, two patients were waiting for screening radiology (68 and 57 days), one patient was considered for a clinical trial that delayed treatment initiation (56 days), and one patient requested a treatment delay (54 days).
Discussion
The Department of Medical Oncology (DMO), University of Pretoria / Steve Biko Academic Hospital only sees patients who have been referred with a histologically-confirmed malignancy. Patients are diagnosed by other departments or institutions and are then referred to the DMO for further treatment.
The median value for the delay between the patient’s first visit to a medical institution and date of biopsy was 90 days ranging from 0 days to 1 260 days. This delay is addressed according to the eight key areas identified in the BCPCP document.2 The eight key areas were developed to streamline a patient’s journey and, in turn, reduce the waiting periods between each consultation. Advocated in this policy is the development of regional and tertiary level specialist breast units (Key Area 2, Objective 5) for the diagnosis and management of breast cancer.2 As of April 2018, there were 26 proposed Regional Breast Units awaiting accreditation, of which eight were situated in the referral areas of the Department, and six Provincial Specialist Breast Units.8 Due to the extremely limited number of qualified, registered Medical Oncologists, reduction in the delay from histology to first consultation and treatment initiation will not be attainable until the training capacity is expanded. While the delays experienced from referral to first consult are not optimal, it must be borne in mind that currently, there are approximately 45 registered, qualified Medical Oncologists in South Africa (one registered Medical Oncologist for more than 1 300 000 people).
Only 15 (19.0%) of patients analysed reported any form of delay due to COVID-19 throughout the study.
Key Area 1: Prevention and early detection, screening and genetic assessment
Early diagnosis of a malignancy leads to an earlier treatment and, ultimately, improved survival rates.9 While screening and breast awareness are of paramount importance to limit the stage of disease at diagnosis, adequate and affordable treatment facilities need to be in place to assist newly diagnosed patients. Richards et al. noted that patients with delays of longer than three months had a shorter survival rate than patients treated in the three months following diagnosis.10
The BCPCP advocates for biannual breast examinations at a primary healthcare clinic and imaged-based screening for high-risk patients.2 Important factors which should precipitate radiological imaging as well as biannual breast examinations at this point include one or more of the following: a previous personal history of breast cancer, a diagnosis of lobular carcinoma, prior radiation at a young age (<20 years old) or prior high dose radiation, BRCA 1 or 2 positivity, family history of breast cancer (first degree relative), and/or having received hormone replacement therapy.
According to the National Cancer Strategic Framework (NCSF) (2017-2022),1 all women attending primary health clinics should be given breast education (printed material and taught self-examination), emphasising that any woman who notices a change in their breasts should contact their nearest medical institution without delay. Women over 40 years of age attending a primary health clinic should have a clinical breast examination biannually. A full breast history and breast examination should be done on all symptomatic women presenting to a clinic / hospital and annual mammograms should be performed from the age of 40. The latter, however, is costly and difficult to book in public hospitals without a prior history of breast cancer. Patients who already access healthcare via the public health sector have a relatively easier and quicker referral than patients who are new to the system. Any patient with a positive finding (confirmatory biopsy) at the regional level should be referred directly to the tertiary / quaternary institution for immediate management and care.
In 2010, the European Society of Breast Cancer Specialists updated their policy statement on the recommended delay times for patients diagnosed with breast cancer. Their recommendations are that patients should not wait longer than six weeks from initial diagnosis to treatment – a time frame, which, they recommended, needed to be achieved in at least 75% of patients.11
In a review of 172 patients diagnosed with breast cancer from KwaZulu Natal, patients were asked the reasons for the delay in requesting treatment. Forty per cent of patients reported that they were not aware that they had cancer, 40% were not aware of the severity of the disease, 40% feared losing a breast, and 34% had difficulty accessing health care.12
While screening (self and/or radiological) was not addressed as a data point in the current study, reasons for delay in seeking medical attention included “too busy” and “did not think it was serious”. One patient delayed seeking medical advice for five months as she performed self-examinations to see if any change occurred. Three patients were sent for further examination after a suspected malignancy was found during a routine follow-up consultation. This speaks directly to Key Area 8, Objective 22, where the role of CANSA and Cancer Alliance is imperative. These organisations are at the forefront of disseminating information to the public on the signs, symptoms, and way forward for all malignant conditions.
Key Area 2: Timely access to care
The BCPCP makes provision for patients to be referred directly to a tertiary / quaternary medical institution for further screening, diagnosis and treatment. Transport assistance from clinics to designated oncology units is mandated in the BCPCP (Key Area 2),2 however, this is dependent on available medically equipped vehicles between the outlying main hospitals and the treating institutions. Patients are still reliant on their own transport from home to the nearest main provincial hospital.
A study undertaken in Soweto reported traveling distance between residence and treating hospital as an important factor in treatment delay, with 45% of patients residing within 10km of the treating hospital, and 95% of patients residing within 50km of the treating hospital (distance was measured as the shortest straight line using global positioning system co-ordinates).13 Of the patients living more than 20km from the treating hospital, 61.8% presented with advanced stage disease.
Total delays experienced by the cohort of patients using public transport ranged from 4-31 months (mean of 12 months), with patient related delays ranging from 0-22 months (mean of seven months), and medical related delays ranging from 1-11 months (mean of four months).
Total delays experienced by patients using private transport ranged from 1-44 months (mean of 12 months), while patient related delays ranged from 0-42 months (mean of eight months), and medical related delays ranging from 1-32 months (mean of four months).
These are similar in times, confirming that the mode of transport did not play a significant role amongst the study’s cohort of patients.
Of the 19 patients with longer delay times, only five patients were reliant on hospital transport. While this figure might seem high for private transport based on the fact that the University of Pretoria is an academic centre within the Steve Biko Academic Hospital (a public hospital), it is important to note that the referral (catchment) areas include parts of Limpopo (LP) and North West (NW) provinces, and the whole of Mpumalanga (MP) and Gauteng (GP) provinces – a total combined population estimated at more than six million. In this study, 4% of the patients were from LP, 2% from NW, 17% from MP and 77% from GP. According to Key Area 2, Objective 5, regional specialist breast units should be set up with a minimum staffing including surgeons, radiology facilities and geneticists; while provincial oncology units require staffing which includes medical and radiation oncologists and sub-specialist surgical services (reconstructive requirements). As of 2018, there were nine specialist breast units operating, with six additional institutions awaiting accreditation. As can be seen by the data, however, these are either not sufficient or operating sub-optimally. There are currently five public hospitals with medical oncology services in Gauteng,14 but a large number of cases are still referred to the two quaternary institutions for management.
Key Area 3: Assessment, diagnosis and staging
Once a suspected symptomatic breast malignancy is identified, a time limit of two weeks for biopsy, histology and radiology results has been set according to the BCPCP.2
In an editorial by Buccimazza published in 2015, delays experienced by patients diagnosed with breast cancer were summarised.15 The reported total delay between initial symptoms and treatment varied between three and four weeks at Groote Schuur Hospital, to between 11 and 19 weeks at Tygerberg Hospital.
In a retrospective cohort of patients diagnosed with breast cancer analysed in South Africa, it was noted that patients experienced a median delay of 21.2 days from biopsy to histology.16 Buccimazza14 reported median delay times between biopsy and final histology of patients diagnosed with breast cancer of less than one week to four weeks across seven hospitals throughout South Africa. All these institutions, however, were reported as having dedicated breast cancer centres.
When considering the proportion of the South African population utilising and accessing the public health services (84%), as opposed to those using private institutions (16%),17 it is understandable that the National Health Laboratory Service would take longer to report on a final histological diagnosis. When the required regional specialist breast units are operational, and with additional, fully staffed laboratory services available, this will prove beneficial to getting results faster.
From the current study, 12 patients had non-representative biopsies, with one patient having undergone three non-representative biopsies prior to diagnosis. Mean delays experienced by patients who had one or more non-representative biopsies was 22 months (range 9-44 months).
While a number of patients did not follow up on their biopsy results, it remains the treating physician’s responsibility to ensure that the patient is informed of the histology result. Patients seen in a public hospital do not retain the initial medical professionals as their primary doctor, which could have led to the definitive diagnosis being delayed.
In patients younger than 35 years of age, breast ultrasound is recommended, whereas in patients older than 35 years of age, mammogram and breast ultrasound is recommended.2
According to the National Institute for Health and Care Excellence guidelines of 2015, any wait for diagnostic tests longer than two weeks for urgent cases and six weeks for non-urgent cases is deemed unacceptable.18
A compounding factor in time delay is availability of radiology facilities. In a report by the World Health Organization: The African Regional Health Report, 201419 reporting on 2013 data, the number of hospitals per 100 000 population was 0.7, with one computerised tomography (CT) facility per 100 000 population; 0.6 radiotherapy units per million population; and 7.8 mammography units per million females (age limit 50 to 69 years).
A mean delay of 21 days from first consultation to final radiology examination was reported in the current study’s cohort of patients. Thirteen patients had their radiology examinations either prior to first consult, or on the same day as their first consult. The mean delay for these patients was nine days, while patients who had their radiology performed after the first consult had a mean delay of 20 days. Treatment was expedited in 10 patients prior to final radiology screening due to the advanced stage of their disease. The delay this cohort of patients experienced is particularly worrisome, highlighting the lack of medical facilities and knowledge about the urgency of suspected malignancy cases throughout the medical fraternity. While the number of institutions visited per patient was 2.5 on average, it is important to note that most public health facilities have all the required specialities within the institution. Private facilities, however, need to refer patients to the public facilities for most of the required laboratory and radiology work needed due to the high costs.
According to the BCPCP, treatment initiation in diagnosed patients with high risk disease should take place within 60 days of first consultation.2 A maximum of 31 days is allowed from the decision to treat, to treatment initiation. In patients with disease requiring adjuvant treatment, treatment initiation following surgery must take place within 60 to 90 days following surgery, while in patients with disease requiring neo-adjuvant treatment, it must be initiated within 30 days of diagnosis.
According to the BCPCP,2 patients should be referred and receive a specialist assessment within 21 to 45 days from first visit (Key Area 2, Objective 5, Standard 2.2). Women presenting with high risk disease should have a specialist assessment within 21 days, while women presenting with low risk disease should be assessed within 60 days (Key Area 2, Objective 6, Standard 2.8)
Mean treatment delay in the study’s cohort of patients was 16 days (range 0-68) with longer delays (>45 days) in five patients owing to a request for treatment delay, a possible clinical study treatment opportunity, and outstanding radiology in two patients. No reason for the delay was given for the remaining patient (delay of 52 days).
Sustainable Development Goal 3 (i.e., the provision of universal health coverage) is directly linked to the proposed National Health Insurance (NHI), with the National Cancer Strategic Framework for South Africa designating between 12 and 60 months to improve on oncology treatment facilities throughout South Africa.1 Another point raised in the National Cancer Strategic Framework for South Africa (point 4(d)) is the Standard Treatment Guidelines which are coupled with the Essential Drug List (EDL) (point 42).20 There is discordance, however, between the BCPCP and the EDL (essential drug list guidelines for public facilities) with certain treatments, i.e., the use of trastuzumab in patients with Her-2 positive disease is recommended for one year by the BCPCP versus six months in the EDL.
Table 3 indicates the difference in policy required time lines versus actual time lines experienced in our patient cohort.
Limitations
Although this study was not planned specifically with the COVID-19 restrictions in mind, they could have played a larger role in delays experienced by the cohort of patients, possibly skewing the results. Also, as this was a single institution study, results may differ from other institutions in terms of patient population, number of medical staff, etc.
Recommendations
The mean total delay time in the study’s cohort of patients from the first symptom to the first treatment of 12 months is concerning. A fast-track system to ensure that patients are sent from their community medical centres to facilities with adequate infrastructure is needed to bring this waiting period in line with the two months mandated in the BCPCP document. Additionally, development and staffing of the promulgated specialist breast units at both regional and provincial level will ensure that patients are diagnosed early and receive optimal treatment to improve quality of life and prolong survival.
Conclusion
Despite the very well-written guidelines relating to patients diagnosed with breast cancer, unless these guidelines are followed and enforced, patients attending public health institutions will continue to be marginalised and experience increased delays between symptoms and treatment.