Introduction
The past 50 years have witnessed extraordinary advances in paediatric oncology care, with survival rates reaching 85–90% in high-income countries.1 Sadly, these advances have not impacted all populations equally; the gap in care has widened as the most vulnerable children have been left behind.2 Ninety percent of the world’s children with cancer reside in low- and middle-income countries (LMICs),3,4 and the large population of children in these regions strains their fragile health systems. Unfortunately, LMICs have less than 5% of the global resources for paediatric oncology.5 Five year mortality from childhood cancer in LMICs is high: nearly 80% of children with cancer die in LMICs, while the mortality in high-income countries is less than 20%.6–9 The World Health Organization (WHO) and St Jude Children’s Research Hospital (SJCRH) launched the Global Initiative for Childhood Cancer (GICC) in 2018. The initiative aims to increase the five-year survival rate of children with cancer from 20% in 2015 to 60% by 2030.10
Childhood cancer is a relatively rare disease but has a disproportionately high number of person-years of life lost in LMICs11 due to late diagnosis and a lack of appropriate referral for treatment, inadequate capacity for diagnostics, therapeutics, supportive, quality of life, long-term follow-up, and palliative care. National cancer control and governmental priorities often neglect childhood cancer.12 However, with improvements in communicable diseases, there is a move to focus on non-communicable diseases, and childhood cancer care has become a global focus.13
In 2022, South Africa’s (SA) total population was 62 million, with 21 million children under 18 years of age, comprising 34% of the total population.14 According to the National Cancer Registry report on childhood cancer, a total of 975 cancers were diagnosed in SA children between 0 and 14 years old in 2018,15 which equates to an overall age-standardised rate of 59.8 cases per million. Similarly, in 2019, 961 cancers were diagnosed in children between 0 and 14 years old, which equated to an overall age-standardised rate of 57.7 cases per million.16 These figures are much lower than those documented in the United Kingdom, Europe, and the United States of America.17,18
The PrOFILE tool
The Paediatric Oncology Facility Integrated Local Evaluation (PrOFILE) tool developed by St Jude Global (SJG) Childhood Cancer Analytics Resource and Epidemiological Surveillance System and the Global Metrics and Performance Unit, is a comprehensive self-assessment tool, used in 25 countries, that allows paediatric haematology and oncology (PHO) facilities and international stakeholders to capture facility-level childhood cancer care data to identify challenges in service delivery and to prioritise solutions locally.19 A systematic assessment of non-biological factors, such as context, facility infrastructure, multidisciplinary care teams (MDT), and communication, provides a better understanding of childhood cancer outcomes in LMICs. Modules covered are national context, facility and local context, diagnostics, finances and resources, service capacity and integration, treatments (chemotherapy, surgery, radiation therapy, supportive care), patient, personnel, and outcomes. The abbreviated PrOFILE version, used in this project, is a 12-module tool that provides an abbreviated, rapid, score-based, and unidimensional PHO facilities assessment. It also aims to promote equity, reduce barriers to PHO care, and integrate with general child health services. The primary data are for the team and facility to use and leverage to improve childhood cancer care delivery. PrOFILE phases lead the team to dynamic prioritisation, emphasising areas amenable to quality improvement and implementation sciences methodologies.
Methods
Institutional PrOFILE evaluations
Each of the 13 public-sector hospitals that treat children with cancer was invited to participate in the PrOFILE evaluation. Each facility identified a physician lead, a site coordinator, and a core group of clinicians to conduct the assessment. The PrOFILE site coordinator and physician lead collected the facility data. Additional questions were directed to the rest of the assessment team to collect the perspective of the point-of-care staff. SJG staff guided the assessment team through general uses for the data collected and how to interpret the site-specific results.
Before the workshop, a team of representatives from the South African Association of Paediatric Haematology Oncology (SAAPHO), the National Department of Health (NDoH), the Childhood Cancer Foundation South Africa (CHOC), WHO, SJG, and national health institutions initiated an assessment, mapping, and evaluation of childhood cancer healthcare delivery in South Africa. The following public-sector hospitals participated in the appraisal: Charlotte Maxeke Johannesburg Academic, Chris Hani Baragwanath Academic, Dr George Mukhari Academic, Frere, Grey’s, Inkosi Albert Luthuli Central, Polokwane Makweng Complex, Port Elizabeth Provincial, Red Cross War Memorial Children’s, Robert Mangaliso Sobukwe, Steve Biko Academic, Tygerberg, and Universitas Academic.
After the data collection, each hospital received two individual reports from SJG: a) a detailed scoring analysis with quantitative data on the unit outcomes, and b) a visual report with tables, graphs, and figures summarising the findings and potential opportunities. All sites then completed a ‘reflections’ analysis based on their institutional reports. Twelve hospitals completed 20 to 30-minute online presentations on their PrOFILE data to their SAAPHO colleagues.
South African National Stakeholder Prioritisation Virtual Workshop
Key representatives from the NDoH, healthcare workers, civil society, international collaborators, and other multi-national implementation stakeholders helped to develop the workshop goal, objectives and deliverables. Approximately 150 participants representing a diverse MDT group of national, regional, and global stakeholders registered and attended.
The workshop convened to forge a robust connection between national priorities and evidence-based assessments, laying the groundwork for achieving several pivotal objectives. Foremost among these was the imperative to furnish key stakeholders with objective assessment data, illuminating the path forward in prioritisation exercises. By anchoring decisions in empirical evidence, the workshop sought to instil confidence in the choices made, ensuring that they were grounded and reflective of pressing needs. It charged the delegates with the crucial task of crafting priorities and action plans to develop a roadmap destined to improve the survival of childhood cancer patients in South Africa. Through meticulous planning and strategic foresight, the workshop aimed to identify focus areas and devise actionable strategies capable of effecting tangible change. Participants hoped to demonstrate SA’s readiness for consideration as a WHO–GICC site. The workshop served as a crucible in which ideas were forged into actionable plans, laying the foundation for a concerted and evidence-driven approach to improve childhood cancer services in the country.
Participants worked in six groups during the workshop, with between 10 and 15 participants per group. Each group was assigned a specific topic, which aligned with one of the six PrOFILE components (context, workforce, diagnostics, MDT, therapy, and patients and outcomes). The workshop consisted of five discrete activities using the Zoom video conferencing platform with breakout rooms and the Mural virtual collaboration platform. Participants were tasked with collaboratively defining ten key priorities to enhance paediatric oncology patient outcomes and experiences across the continuum of care.
The SJG facilitators provided an overview of the PrOFILE exercise. Six groups of participants reviewed the PrOFILE recommendations, utilising a categorisation exercise to help participants identify five initiatives from the recommendations for implementation. Participants categorised each recommendation into one of three groups: (1) the country (SA) is currently working on it; (2) the country is not working on it but it is essential to start; or (3) the country is not working on it and does not have the resources to do so right now.
Results
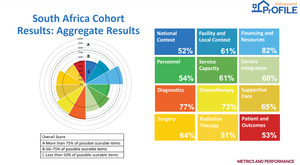
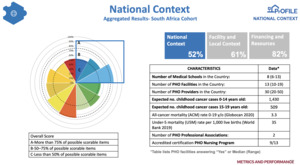
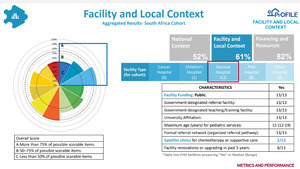
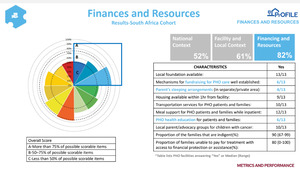
The National Aggregate PrOFILE report
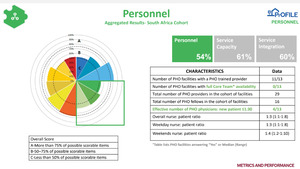
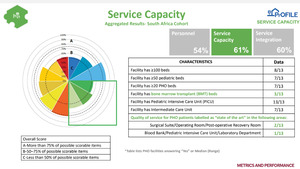
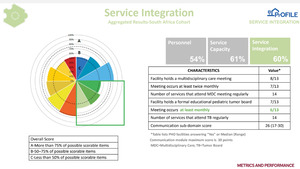
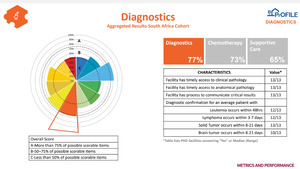
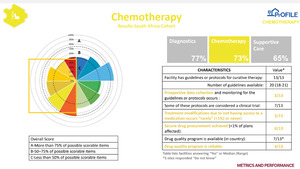
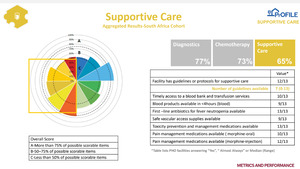
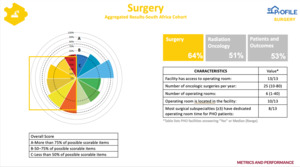
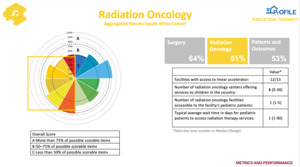
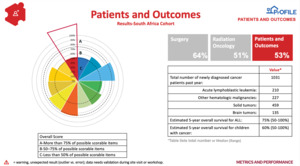
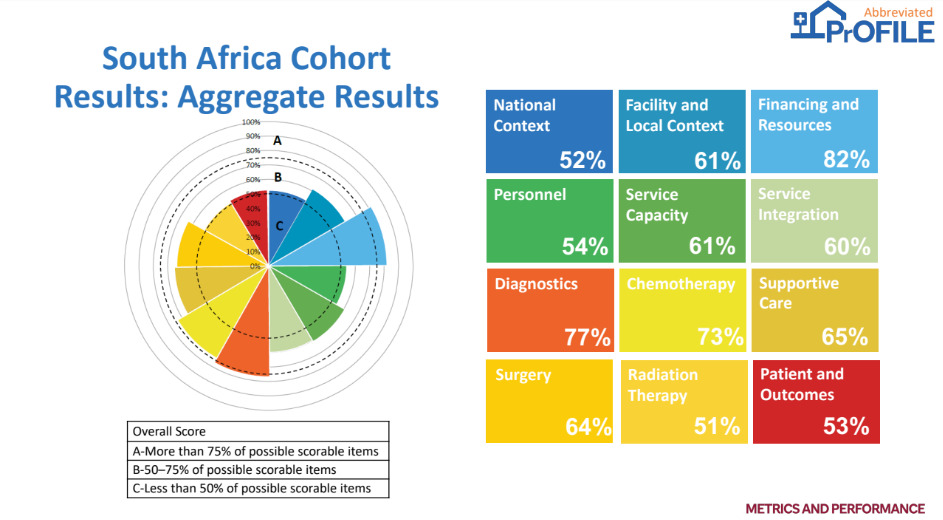
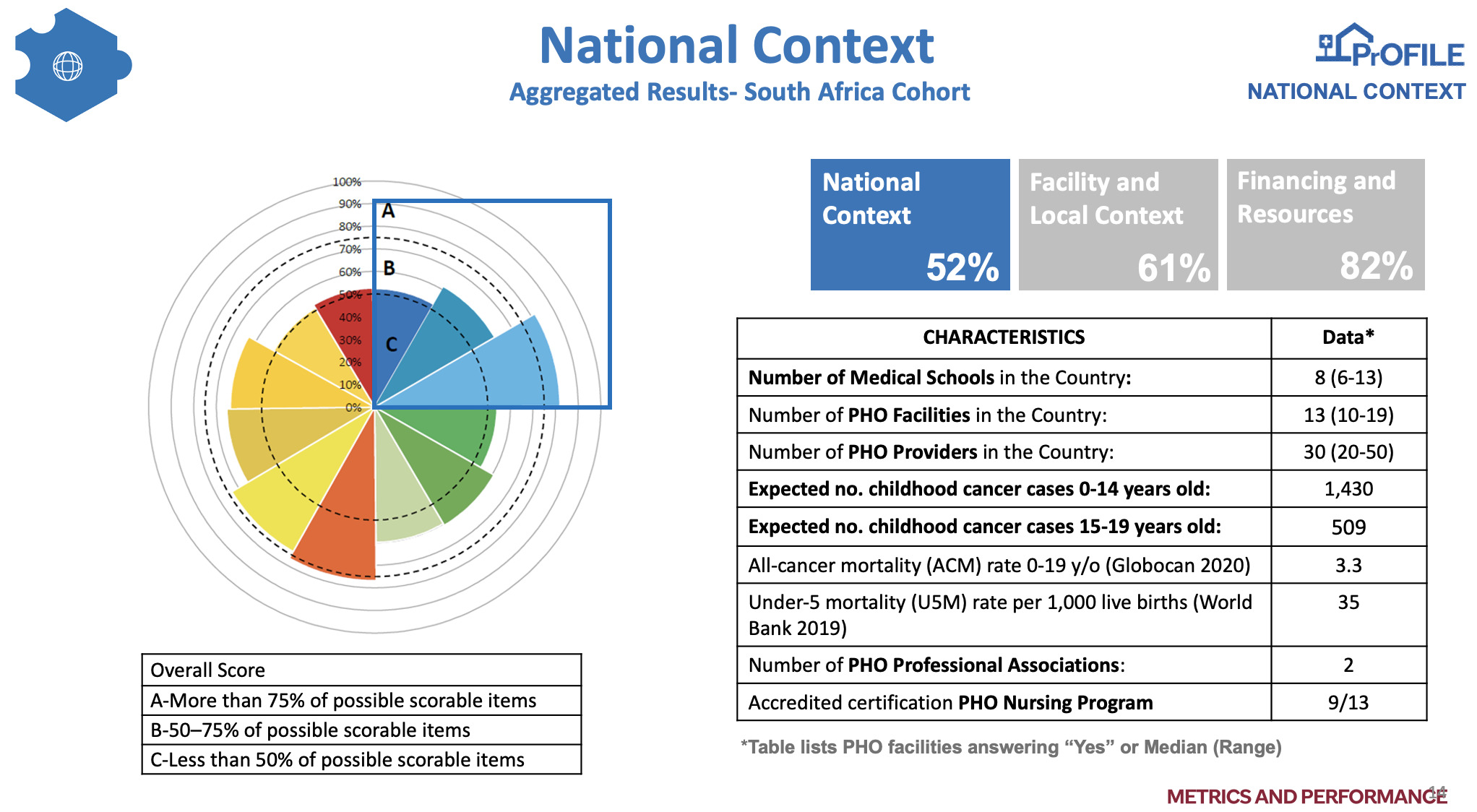
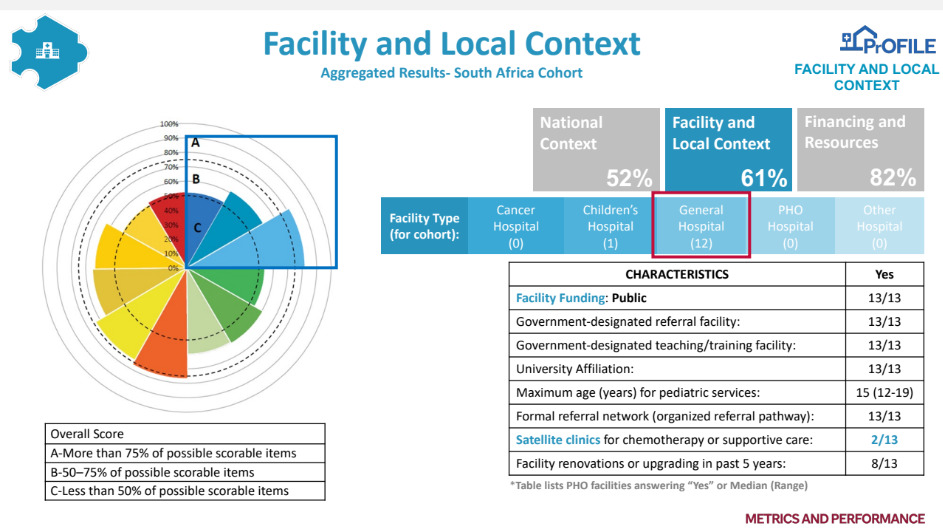
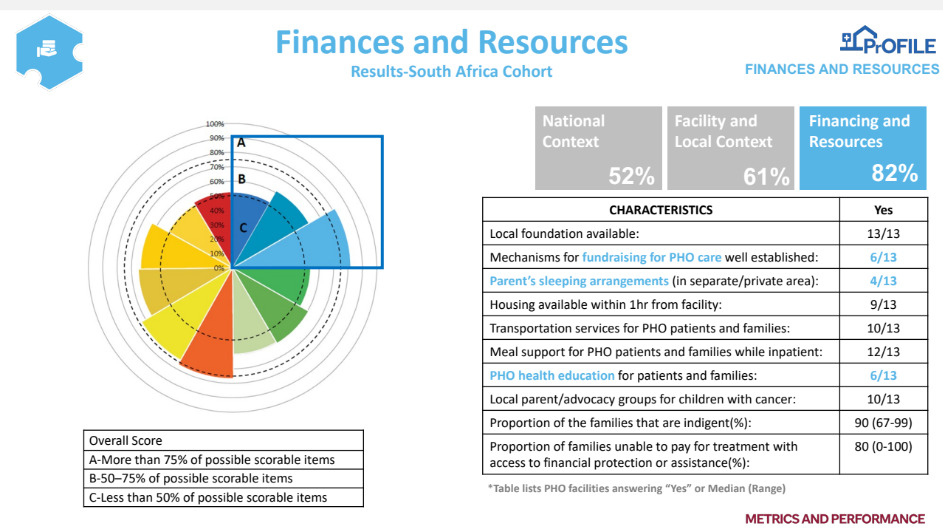
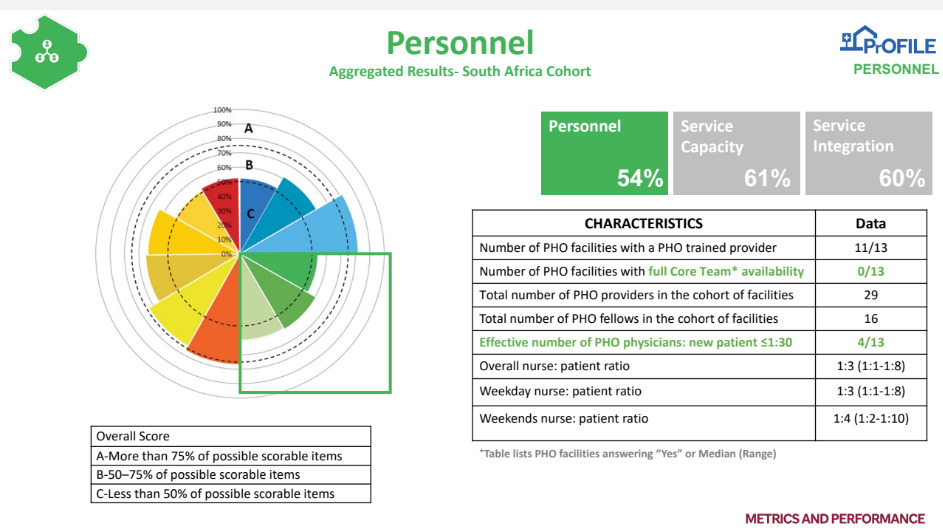
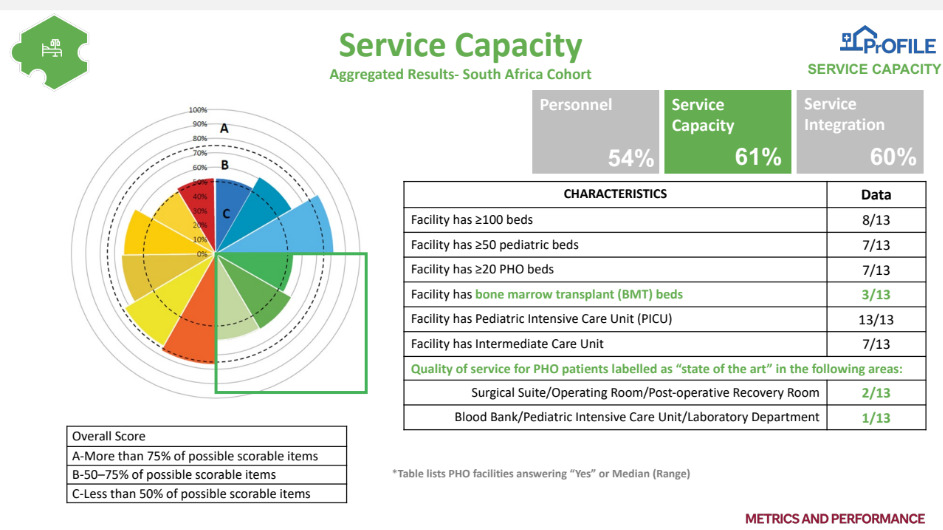
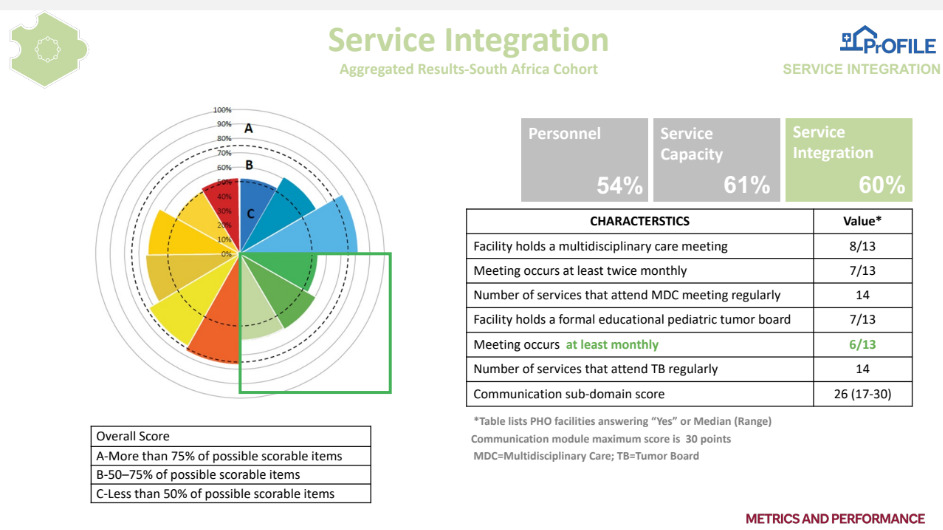
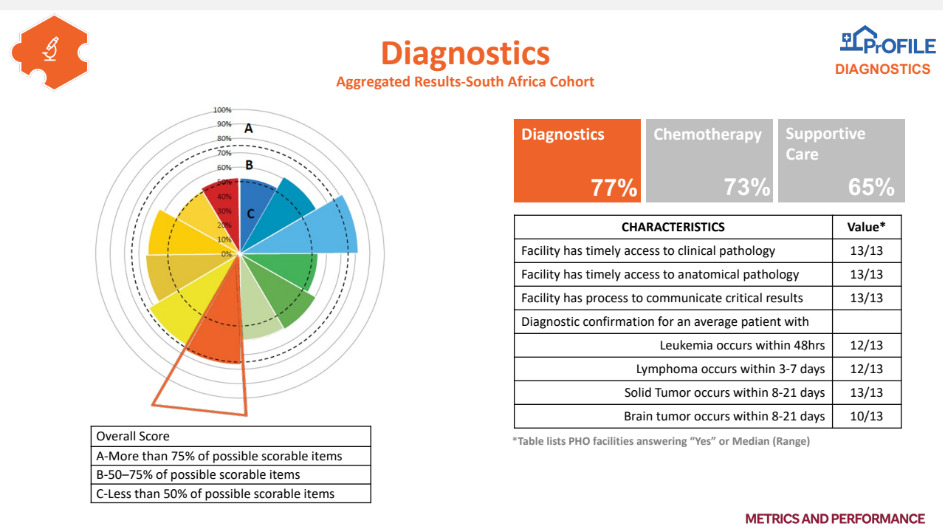
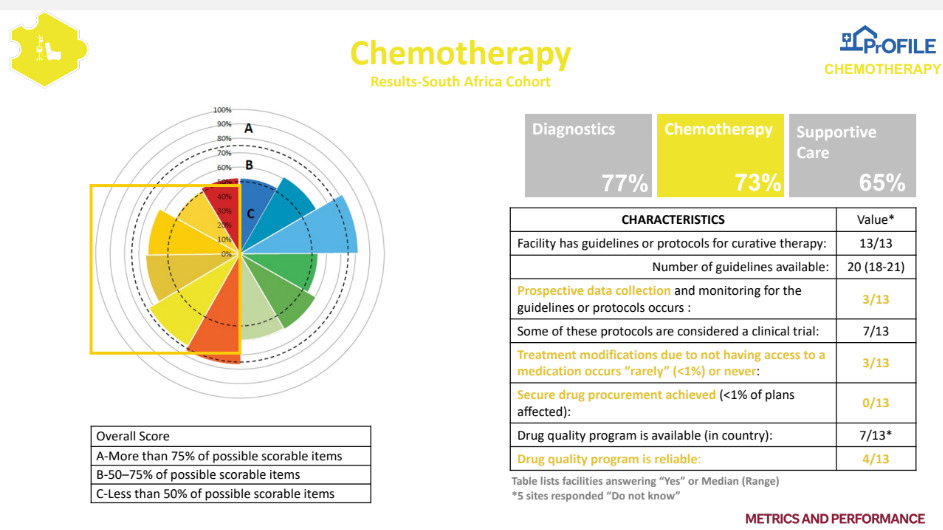
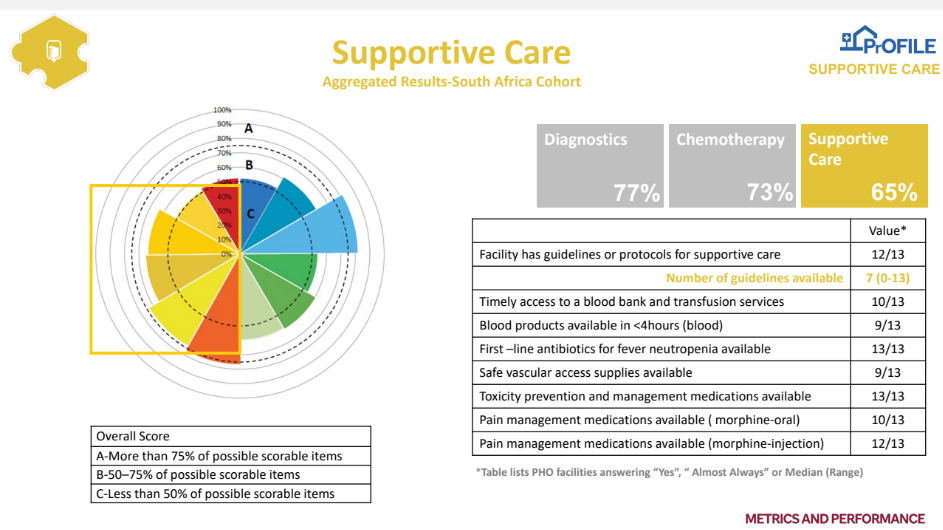
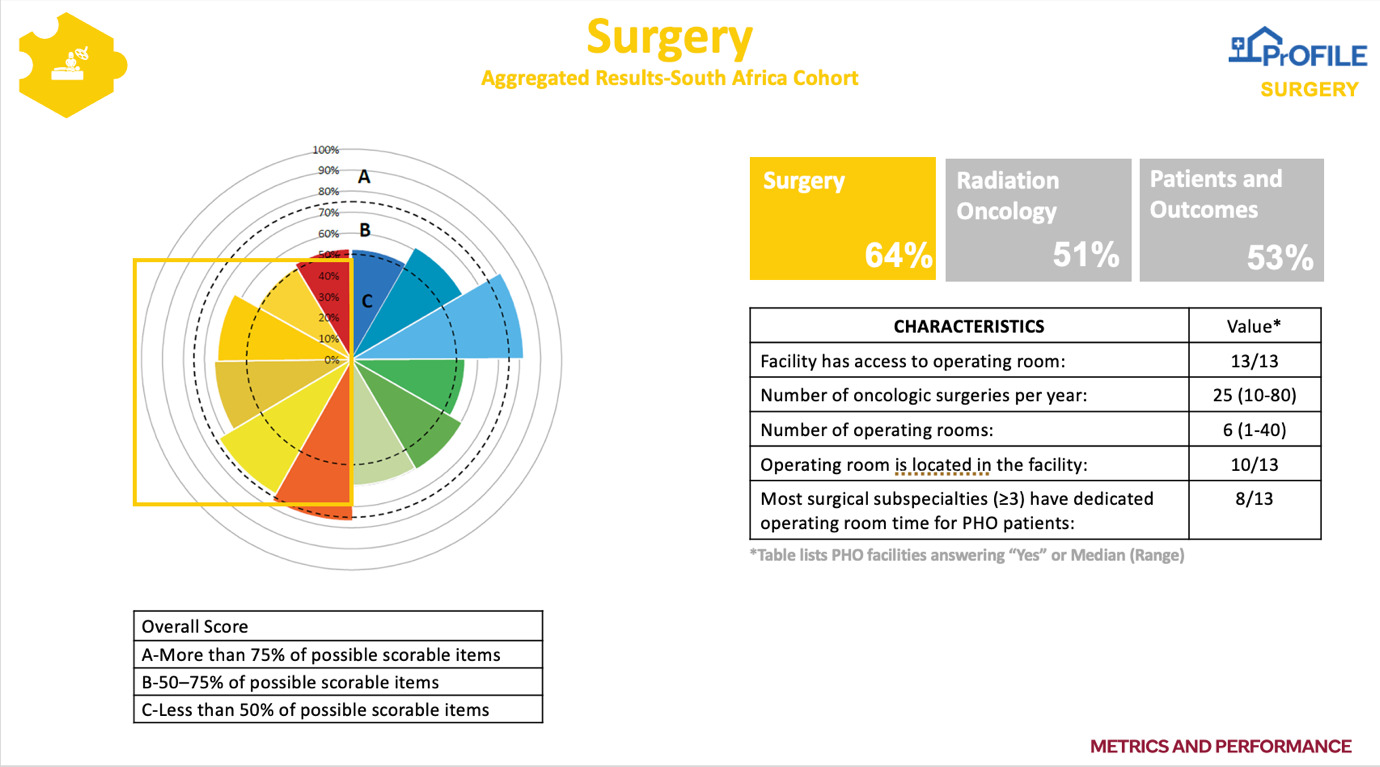
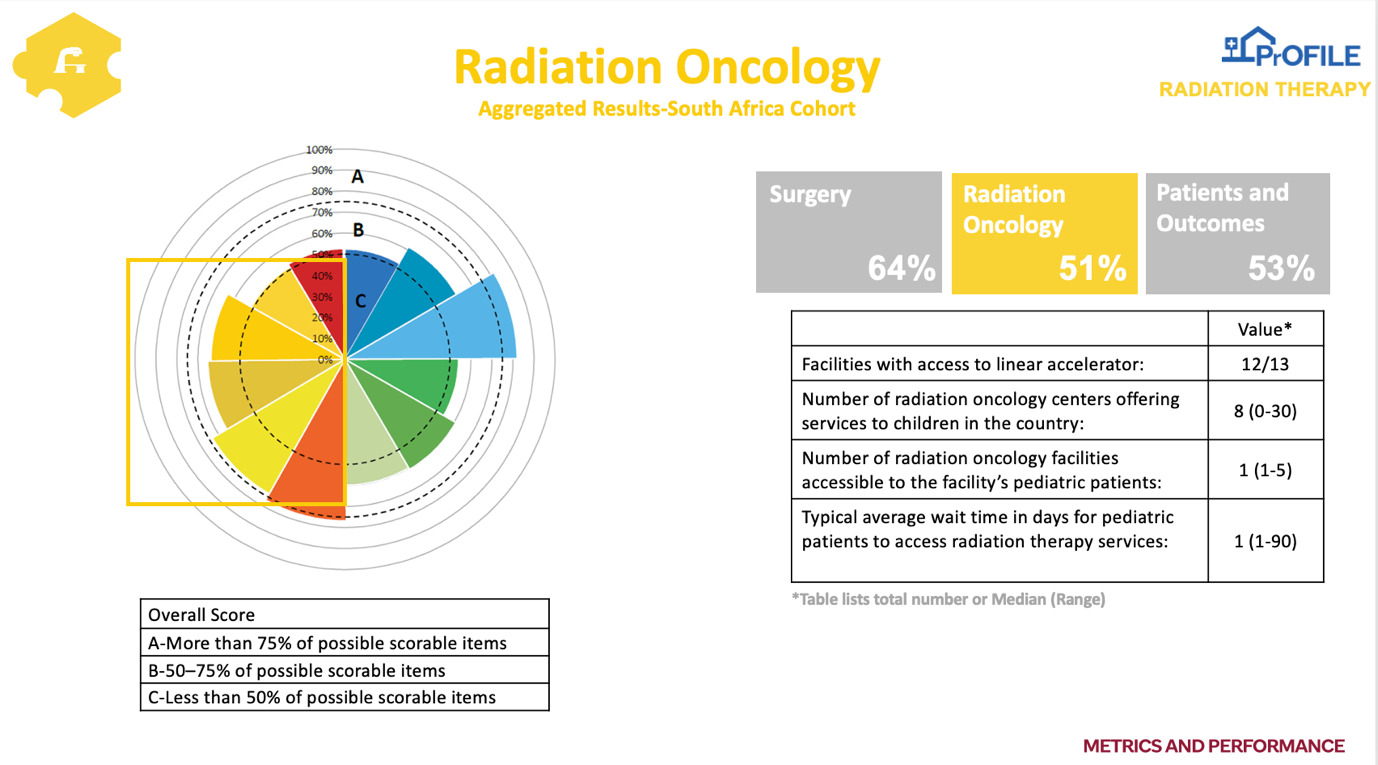
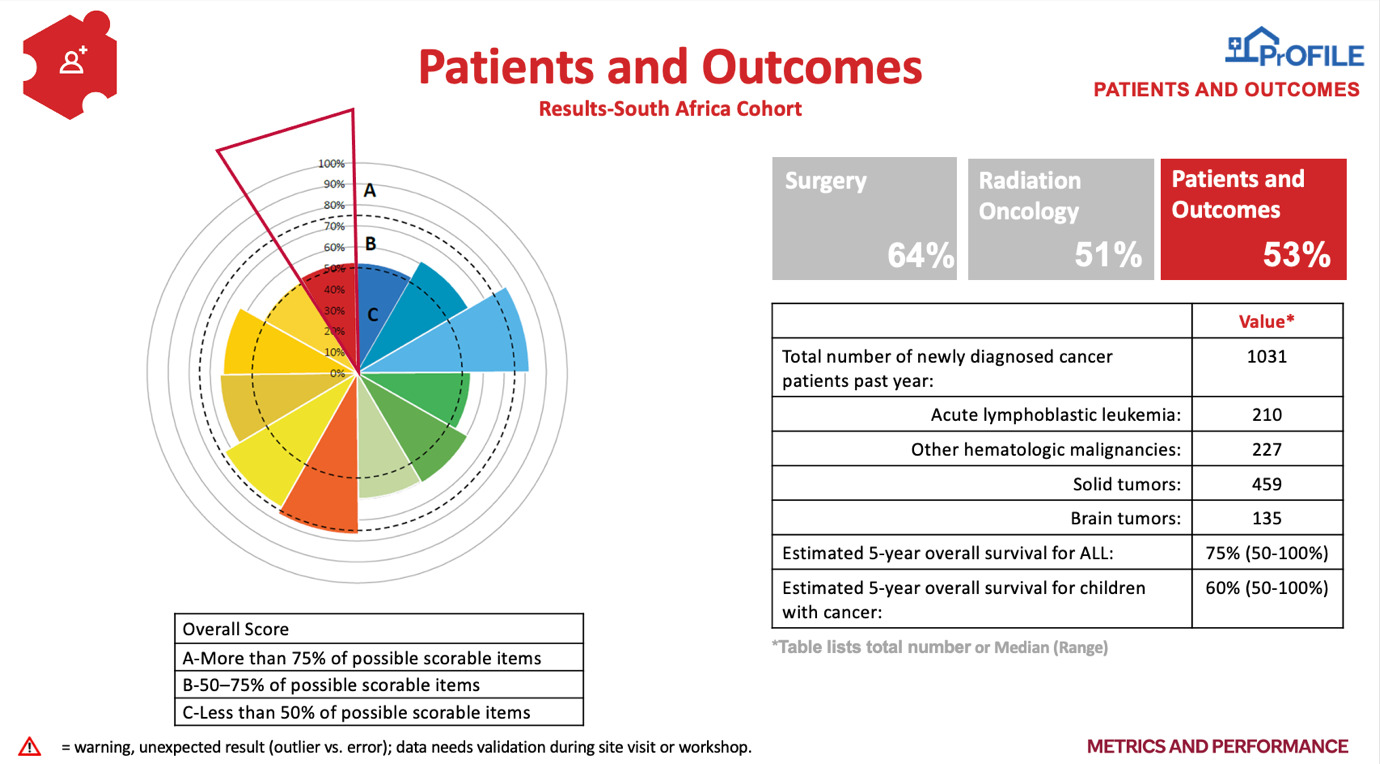
In addition to the individual hospital reports, a national aggregate report (Figures 1 and 2) was compiled and used as the basis from which to discuss opportunities and priorities at the workshop. Evidence from the aggregate PrOFILE report was compiled and summarised for all participants. Results of national context (Figure 3); facility and local context (Figure 4); finances and resources (Figure 5); personnel (Figure 6); service capacity (Figure 7); service integration (Figure 8); diagnostics (Figure 9); chemotherapy (Figure 10); supportive care (Figure 11); surgery (Figure 12); radiation oncology (Figure 13), and patients and outcomes (Figure 14) were distributed to all participants before the virtual workshop.
Categorisation exercise - mapping of current and planned activities
Each working group mapped current and planned activities. Groups focussed on several priority areas, including increasing local fundraising, upgrading inpatient care areas at PHOs, enhancing access to paediatric subspecialists, and improving access to financial assistance for at-risk services like medical supplies and housing. In addition, efforts underway to increase the impact of awareness campaigns and foster international collaborations were identified. Key initiatives included upgrading parent sleep spaces, addressing diagnosis delays due to reliance on traditional, complementary, and alternative medication, improving procedural pain management, and enhancing parent education. Furthermore, the need for cyclic accreditation of PHO facilities was established, as were improving the national healthcare infrastructure and ensuring continuity of care in general paediatrics, especially regarding benign illnesses and cancer survivorship.
Workforce enhancements involved increasing fever and neutropenia care in emergency rooms, strengthening PHO teams, and bolstering professional nursing staff, alongside initiatives to improve hand hygiene and PPE availability. Diagnostic improvements focussed on enhancing access to specialised laboratories, improving communication during diagnostics imaging, and ensuring timely reports. The focus of MDT care efforts was to increase surgery resources, improve surgical reports, enhance the timeliness of services like radiotherapy, and prioritise PHO surgery. Chemotherapy and supportive care initiatives included standardising protocols, strengthening safety practices, and increasing drug access and supportive care services. Patient outcomes were targeted through prospective data collection, upfront palliative care services, tracking and reducing time to antibiotics, and optimising treatment initiation with curative intent, all aimed at improving long-term outcomes and the publication of results.
Prioritised recommendations
The recommendations from the virtual workshop are presented in Table 1. The five prioritised recommendations outlined by the working groups encompass a comprehensive strategy to enhance paediatric healthcare across various domains.
The five projects identified are: 1. To strengthen a hospital-based tumour registry for childhood cancer and to develop a paediatric population-based registry; 2. To develop national chemotherapy safety guidelines and standard operating procedures to ensure the safety of chemotherapy administration; 3. To complete the febrile neutropenia guidelines for South African children with cancer, publish the manuscript on the guidelines, implement the febrile neutropenia guideline, develop a protocol to improve the time to antibiotic administration for the child on cancer treatment and febrile neutropenia, and record the data in the SJCares Fever Registry; 4. To standardise multi-disciplinary team reporting with the aim of developing standardised and consistent reporting of surgical procedures, radiology, pathology, and radiation oncology reports for children with cancer, and 5. The development of national protocols – in addition to ALL – protocol development should be prioritised according to the WHO-GICC six index cancers in children. The focus on continuity of care underscores the importance of seamless transitions for patients, whether in general paediatrics or cancer survivorship, alongside establishing satellite clinics to ensure accessibility and convenience.
Moreover, initiatives to bolster internet connectivity within hospital settings and for patients themselves reflect a recognition of the role of technology in facilitating communication and access to information. Concurrently, efforts to increase awareness of national cancer control programmes and to secure additional research funding signal a commitment to advancing treatment modalities and improving outcomes in paediatric oncology. The workforce-related recommendations emphasise the necessity of a well-supported and patient-centric healthcare team, from assuring posts for public health organisation providers to integrating patients and families into treatment decisions. Enhanced diagnostics, MDT care, and standardised chemotherapy protocols across the country underscore a holistic approach to paediatric treatment, ensuring timely and comprehensive interventions tailored to each patient’s needs. Finally, the focus on patient outcomes encompasses initiatives such as upfront palliative care services and data-driven strategies to reduce early mortality rates, reflecting a dedication to improving the quality and longevity of paediatric healthcare outcomes. Together, these prioritised recommendations offer a roadmap for optimising childhood cancer care delivery and fostering positive outcomes for young patients and their families.
Collaboration analysis
The delegates performed a collaboration analysis to identify critical challenges to implementing the categorisation exercise recommendations. Participants identified potential solutions to these challenges as well as national and international collaborators. In the realm of childhood cancer care, the journey from diagnosis to survivorship is rife with challenges, notably in ensuring continuity of care across the spectrum of illnesses, from benign conditions to cancer survivorship. Infrastructure deficits, such as the need for more standardised laboratory testing and limited access to specialised diagnostics, hinder timely diagnosis and treatment initiation. Moreover, transitioning paediatric patients into the adult healthcare system poses a significant challenge, requiring the development of individualised care plans, guidelines for late effects, and seamless collaborations between paediatric and adult practitioners. Addressing these challenges necessitates local efforts and international collaborations, leveraging the expertise of institutions like SJG and partnerships with United Nations agencies and disease-specific non-governmental organisations to enhance diagnostic capabilities, streamline treatment protocols, and improve patient outcomes.
On the workforce front, shortages of trained healthcare workers and nurse educators exacerbate the existing workforce crisis, necessitating innovative solutions such as offering speciality training at nursing colleges and benchmarking between units to ensure optimal staffing levels and competencies. Financing mechanisms include funding support from international partners and twinning programmes with institutions in other countries to alleviate financial constraints and facilitate the recruitment and retention of skilled professionals in PHOs. Moreover, sensitisation efforts and incident reporting systems will promote retention and enhance the quality of care by identifying and addressing workforce-related issues.
Increasing access to specialised laboratories and standardising testing procedures are paramount in diagnostics. Collaborations are required between local hospitals, the private sector, and international organisations to improve infrastructure, reduce turnaround times, and ensure cost-effective testing modalities. Clear communication channels and national standards for laboratory testing are essential for streamlining reporting results and patient identification, facilitating timely interventions, and improving overall diagnostic efficiency.
To strengthen chemotherapy safety practices, robust training programmes are imperative for pharmacists and nurses, as are implementing standardised operating procedures and spill kits. International platforms like SJG and SIOP Africa e-learning can disseminate best practices and enhance training opportunities for healthcare professionals.
Finally, improving prospective data collection and electronic database management is critical for advancing research and improving patient outcomes in childhood cancer. Standardising data collection processes, fostering collaborations between units, and leveraging user-friendly platforms can streamline data management and facilitate knowledge sharing, ultimately enhancing the quality of care and driving innovation in childhood cancer globally.
Ensuring continuity of care and optimising outcomes for young patients presents a multifaceted challenge. Various obstacles, including infrastructure limitations, workforce shortages and fragmented care, hinder seamless care provision. Strategic recommendations and innovative solutions are needed to improve the overall quality of paediatric oncology services.
Impact-effort matrix
The working groups used an impact-effort matrix to identify the projects to be implemented based on areas amendable to improvement. The impact-effort matrix weighs the impact of each solution against the effort required for implementation, allowing groups to identify ‘low-hanging fruit’ or projects that have high impact and require low effort. Participants voted for the top two recommendations from the five groups based on their impact-effort scores. Each group assigned impact and effort scores to their five prioritised recommendations.
Discussion
Action plan and timelines
The virtual workshop participants outlined several priority projects to enhance paediatric oncology care across various domains. One key initiative involves developing comprehensive care plans and transition curriculums for paediatric oncology survivors to ensure seamless continuity of care as they transition from PHO services to general paediatric or adult care. This initiative includes milestones such as stakeholder engagement, assessment of existing resources, curriculum development, and a pilot programme launch.
Another vital project focuses on establishing satellite clinics in regional hospitals to provide essential services for benign haematology and active cancer patients requiring therapy, thus alleviating the burden on families and clinics. This endeavour involves identifying referral centres, stakeholder engagement, curriculum development, training, and launching a scalable pilot programme.
Regarding workforce development, the group aims to support nursing education in PHOs and to increase the number of trained nursing staff by 25% in the short term, which will entail conducting a situational analysis, obtaining buy-in from authorities and stakeholders, developing a curriculum, pilot testing, accreditation, and implementation.
To ensure adequate staffing for PHO providers, the group plans to define benchmarks and strategies to achieve 75% capacity of provider posts within the next few years, involving stakeholders and obtaining approval from relevant health authorities.
Efforts are underway to improve MDT communication during imaging diagnostics by developing a national scorecard and local communication expectations, with milestones including leadership engagement, stakeholder involvement, and measurement of communication success. Moreover, initiatives are being pursued to enhance the timeliness of pathology reports and radiation therapy services, with milestones including audits, stakeholder engagement, and establishing reporting systems and communication channels.
In chemotherapy and supportive care, the focus is on improving access to essential drugs and establishing end-of-life care services through procurement processes, stakeholder engagement, funding acquisition, recruitment, and the development of standard operating procedures.
Finally, initiatives to increase prospective data collection and reduce early deaths through timely antibiotic administration involve consensus-building, data infrastructure development, training, and implementation of standardised protocols.
These comprehensive projects underscore the commitment of the working groups to improving childhood cancer care through multifaceted interventions addressing workforce development, infrastructure, diagnostics, MDT, treatment protocols, and data management.
Themes for advancing paediatric oncology care
The PrOFILE working group identified several vital themes for advancing paediatric oncology care in South Africa. Firstly, there is a strong emphasis on integrating MDT perspectives and implementing shared care models, leveraging the expertise of various healthcare professionals, including surgeons, radiation oncologists, radiologists, palliative care specialists, pharmacists, pathologists, and nurses. Collaboration with the government is crucial to ensure equitable provision of necessary posts to address the workforce shortages. In addition, decentralising shared care models and survivorship transition to peripheral health centres aims to make healthcare more accessible to families, focusing on empowering nurses as frontline workers through enhanced educational opportunities.
Secondly, the group highlighted the importance of addressing quality of care by establishing comprehensive guidelines and protocols. National policies are essential for informing various aspects of cancer care, from infection management to palliative care and survivorship. The aim is to enhance the overall quality of care by avoiding duplication of efforts, identifying existing stakeholders, and efficiently allocating resources.
Finally, the PrOFILE working group emphasised the need to foster a culture of continuous improvement through data-driven initiatives to tackle timeliness and communication gaps through targeted quality improvement projects, particularly in areas like pathology and diagnostic imaging. Investing in prospective systems for practice change across all centres in South Africa and providing training opportunities in quality improvement and implementation science were also proposed to ensure sustained progress in cancer care delivery.
These themes underscore the importance of collaboration, standardisation, and ongoing innovation in advancing cancer care in South Africa. The goal is ultimately to improve patient outcomes and experiences across the continuum of care.
Recommendations
After analysing priorities identified through workshop participation and thematic exploration, the NDoH, SAAPHO, South Africa WHO Country Office, and SJG recommended several strategic next steps. A priority is to establish a dedicated structure within the NDoH framework to strengthen efforts in paediatric oncology control, aiming to achieve the WHO-GICC goals by following the guidelines and recommendations set forth by the WHO-GICC for the six index cancers. This will help to sustain progress, coordinate policy activities, and aid in budgetary planning for effective initiative implementation. The committee will include diverse stakeholders both within and outside the NDoH to ensure comprehensive representation. Formalising collaboration through letters of intent or memorandums of understanding with relevant partners is essential to advancing the identified initiatives. There is advocacy for the reform of SAAPHO’s governance structure to align with the identified priorities and themes, encouraging the engagement of MDTs and participation in various academic projects.
Enhanced engagement with the WHO Regional Office is recommended, including submitting workshop results to the South Africa WHO Country Office and seeking formal technical support to address key collaboration areas. This approach aligns with implementing the South African National Health Institution Bill, which aims to provide a legal framework for establishing and functioning national health institutions in South Africa. Addressing funding, performance management, and oversight ensures that national health institutions operate effectively and align with national health goals. This will help to sustain progress, coordinate policy activities, and aid in budgetary planning for effective initiative implementation.
Conclusion
The PrOFILE tool enabled a comprehensive evaluation of health services delivery for childhood cancer patients in public sector hospitals in SA. The subsequent national stakeholder prioritisation virtual workshop brought together a diverse MDT of people, who collectively developed actionable plans, the success of which is demonstrated by the active implementation of the priorities identified by the workshop’s working groups. Based on mapping and outputs from the PrOFILE workshop, the NDoH will facilitate the creation of a childhood cancer committee to sustain progress on the key themes and priorities identified through the PrOFILE mapping process. This collaborative approach aims to overcome barriers and drive effective implementation of paediatric oncology control strategies in South Africa with the overall aim of improving the survival of children with cancer.