Introduction
In his acclaimed book, The Emperor of All Maladies: A Biography of Cancer,1 Siddhartha Mukherjee powerfully reminds us that cancer is not a singular disease but a collection of many, aptly describing it as “the defining plague of our generation”1(p18) and a “lethal shape-shifting entity imbued with… penetrating metaphorical, medical, scientific, and political potency.”1(p18) Mukherjee’s characterisation underscores the complex and multifaceted nature of cancer, which continues to pose significant challenges to healthcare systems around the world.
The South African Health Review 2023 (Review) focuses on examining the successes, challenges, and gaps in cancer treatment and care within the South African healthcare system. Central to this examination is the National Cancer Strategic Framework 2017–2022 (NCSF), the current guiding policy document for cancer control in the country. Despite its outdated status, the NCSF remains a critical framework for understanding and addressing cancer care in South Africa.2
The NCSF highlights the importance of the National Cancer Registry (NCR), established in 2011, and the subsequent regulations under the National Health Act of 2003, which mandate the reporting of confirmed cancer diagnoses. However, the strategy also exposes significant deficiencies in the availability of comprehensive data on the cancer burden in South Africa. For instance, while the strategy notes that cancer-related deaths account for approximately 9% of all-cause mortality in adults, it fails to provide data on cancer mortality among adolescents and children. Furthermore, the NCSF underscores the persistent inequities in access to cancer care, particularly affecting “black Africans, poor, uninsured, and rural residents.”2(p9) These gaps highlight the urgent need for updated policies and more inclusive cancer care initiatives to ensure equitable access and improved outcomes for all South Africans. The next section presents the cancer indicators, focusing particularly on the cancer profile for South Africa, as captured from international databases such as the Global Cancer Observatory and the local databases such as the NCR and webDHIS.
Cancer indicators
The World Health Organization (WHO) defines cancer as a large group of diseases that can affect any part of the body, also known as neoplasms or malignancies.3 Cancer incidence is rising globally and locally in South Africa, with cancer being the second leading cause of global mortality.4 The burden of cancer on the African continent is expected to double in the next 20 years as the population ages, where currently, cancers account for 10-20% of morbidity.5
Global Cancer Statistics 2020 (GLOBOCAN) provides estimates of cancer incidence and mortality across 185 countries.6 In 2020, there were an estimated 19.3 million new cancer cases and almost 10.0 million cancer deaths worldwide. Female breast cancer was the most commonly diagnosed cancer, responsible for an estimated 2.3 million new cases in 2020, followed by lung, colorectal, prostate, and stomach cancers. Lung cancer remains the leading cause of cancer death, accounting for an estimated 1.8 million deaths globally. The global cancer burden is expected to reach 28.4 million cases in 2040.5,6
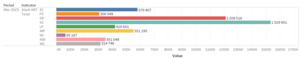
The International Agency for Research in Cancer (IARC) is the driving force behind the Global Initiative for Cancer Registry Development (gicr.iarc.fr), a collaboration of leading cancer prevention organisations that aims to address data availability while ensuring the reliability of cancer incidence data by enhancing their quality, comparability, and use. Data collected in this framework is available through IARC’s GLOBOCAN database. The estimated number of cancer cases and deaths from 2002 through 2018 is available at the Global Cancer Observatory (http://gco.iarc.fr). In assembling regional and global profiles, the GLOBOCAN methods for incidence and mortality estimation rely on the best available data from a given country.7 The Global Cancer Observatory provides access to updated figures at a national level.8 The 2022 South Africa fact sheet reported 111 321 new cancer cases in 2022, 282 418 prevalent cases and 64 547 cancer deaths.9 Data from the NCR, for 2015 to 2022, are shown in Figure 1, Figure 2 and Figure 3. In the South African context, the most commonly diagnosed cancers in women are breast, cervical, skin and colorectal cancer. Similar to the global context, the most common cancers in males in South Africa are prostate cancer along with skin, colorectal and lung cancers.4
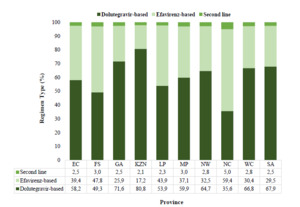
Despite recent initiatives aimed at improving cancer epidemiology in Africa, data on cancer rates remain fragmented and are often dispersed across multiple registries, making comprehensive analysis challenging.7 In South Africa, where the cancer incidence rate is notably high, the situation is further complicated by a significant lack of up-to-date, reliable data. The most recent data published by the NCR covers only up to 2022, leaving a substantial gap in our understanding of the current cancer burden. This lack of current data poses serious challenges to assessing the prevalence and impact of cancer in the country accurately. Without timely and comprehensive data, it becomes difficult to monitor trends, allocate resources effectively, and develop targeted interventions. Figure 1, which illustrates the number of cancer diagnoses among males and females in South Africa from 2015 to 2022, underscores this issue. While the figure provides some insight, it is widely believed that the numbers represented account for only a fraction of the actual cancer cases in the country.
There are significant concerns about the underreporting of cancer cases, which can be attributed to several factors. One major issue is the misattribution of death causes, where cancer is often not recorded as the primary cause of death, leading to inaccurate mortality statistics. Additionally, underreporting by medical facilities, due to insufficient training or inadequate reporting systems, further contributes to the data gap. Another critical limitation is the NCR’s reliance on pathology-based diagnoses, which excludes cases where cancer is diagnosed clinically or radiologically but not confirmed through pathology. This restriction means that many cancer cases, particularly in regions with limited access to pathology services, are not captured in the official statistics.
The cumulative effect of these factors is a substantial underestimation of the true cancer burden in South Africa. This underreporting hampers the ability of public health authorities to understand fully the scope of the problem, design effective cancer control programmes, and evaluate the success of existing interventions. To address these challenges, there is an urgent need to improve cancer data collection and reporting mechanisms, expand the scope of the NCR to include non-pathology-based diagnoses, and ensure that all healthcare facilities are equipped and mandated to report cancer cases accurately and consistently. Only with more reliable and comprehensive data can South Africa hope to combat the growing cancer epidemic effectively and improve outcomes for all affected individuals.
In 2023, Statistics South Africa (Stats SA) produced a report10 with a specific focus on cancer occurrences and their contribution to morbidity and mortality in South Africa. The report illustrates the trends over time and outlines their burden on each population group and age group between 2008 and 2018. Stats SA found that, in 2018, cancer and benign tumours accounted for 9.7% of all mortality in the country, making these the fourth leading cause of death.
Cancer profile in South Africa

Figure 1.Number of diagnoses among males and females, 2015-2022
Source: National Cancer Registry, 2024.11

Figure 2.The most diagnosed cancers by site, 2022
Source: National Cancer Registry, 2024.11
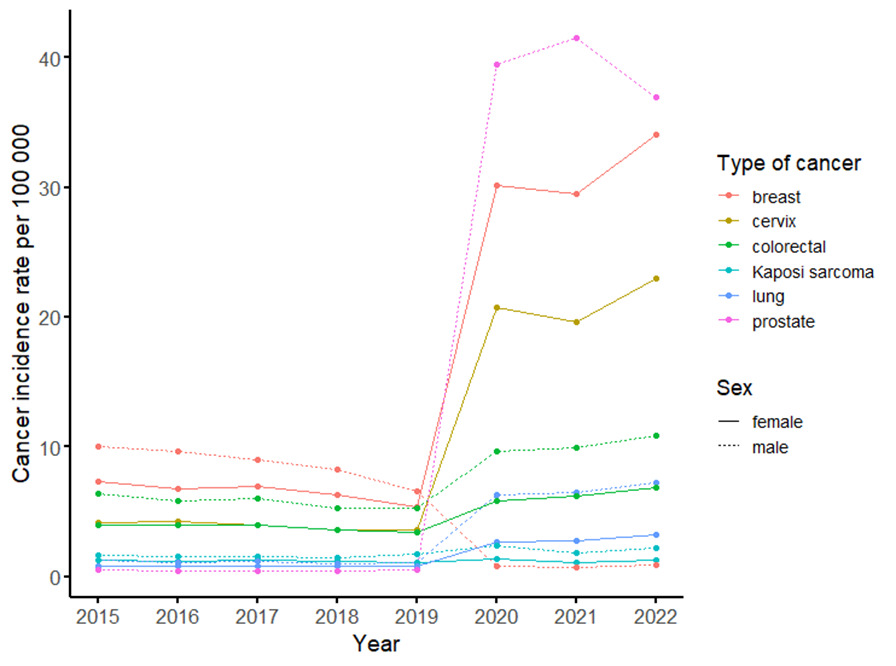
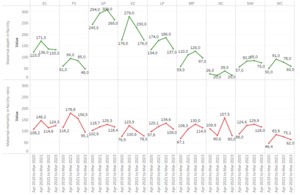
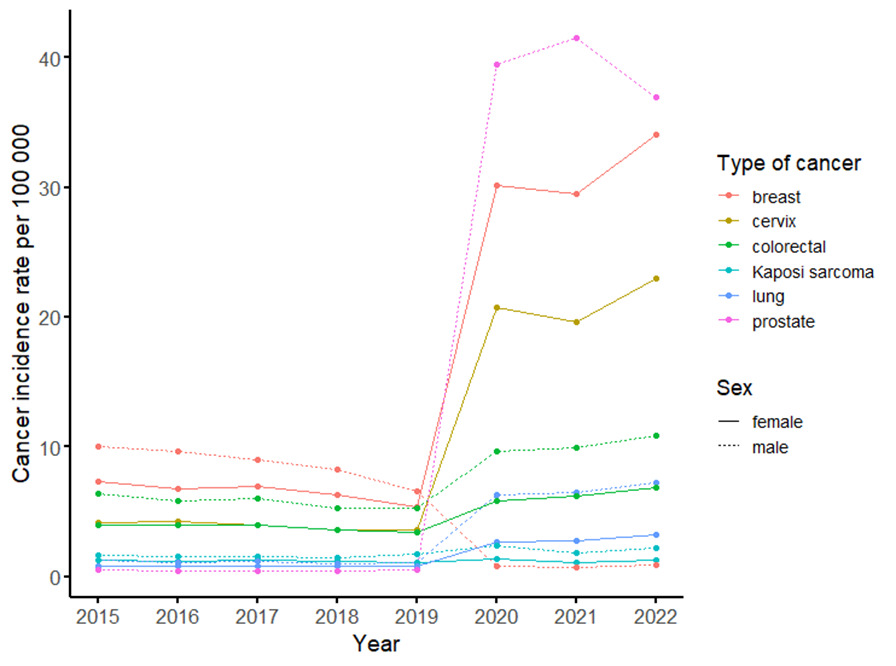
Figure 3.Cancer incidence rate by type of cancer per 100 000 population, 2015–2022
Source: National Cancer Registry, 2024.11
Figure 3 presents cancer age standardised incidence (per 100 000) by sex and type of cancer among the top three invasive cancers in the South African male and female populations.12 Across all cancers presented in Figure 3, cancer burden in males increased sharply from the year 2019 for prostate, colorectal, and lung cancers. However, a reduction in incidence was seen post-COVID-19 for prostate cancer only, while colorectal and lung cancer continued to increase. Male breast cancer incidence declined consistently from 2015 through 2019 and then increased sharply to 2022. The highest burden in females was seen during the COVID-19 pandemic period, where breast, cervical, and colorectal cancer presented with the three highest incidences per 100 000, respectively. Surprisingly, unlike the male cancers, female cancer incidences did not decline post-COVID-19. The apparent increases in new cancer cases could possibly be due to the reported decline in cancer diagnostics during the pandemic. A study to assess the impact of COVID-19 on cancer diagnostic services in 2020 in the Western Cape, found declines in six major histopathological diagnoses.12 Substantial declines were seen for prostate, oesophageal, breast, gastric, and colorectal cancer. The smallest decline was seen in cervical cancer. These data, although generated from a single context, along with the current trends of the top three most invasive cancers, show evidence of the impact caused by national disruption of cancer diagnostic services as result of the pandemic. Additional efforts are required to optimise diagnostic services, ensuring timely initiation of treatment.
Cancer and Kaposi sarcoma
The high prevalence of HIV in South Africa necessitates an understanding of the burden of cancer associated with HIV. The age-adjusted incidence rate (per 100 000) trends from 2015 to 2019 remained consistent, reaching a peak in 2020 before reverting to the pre-COVID-19 trends in 2021, as per data from the NCR. Throughout this reporting period, males consistently demonstrated a heavier burden than females. Furthermore, a record linkage study, which evaluated the burden and association between HIV and cancer during the decade of 2004-2014, reported that 30 487/46 951 (65%) of all female cancer cases and 16 443/46 951 (35%) of all male cancer cases were among people living with HIV (PLHIV).13 Altogether, PLHIV were at higher risk of AIDS-defining cancers compared to HIV-negative patients. Collectively, the incidence of Kaposi sarcoma, and other AIDS-defining cancers needs to be monitored in PLHIV.
Cancer programme coverage in Africa
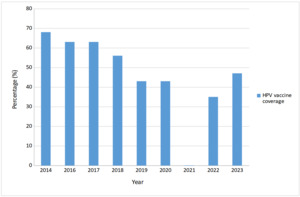
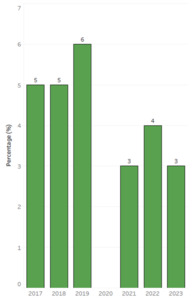
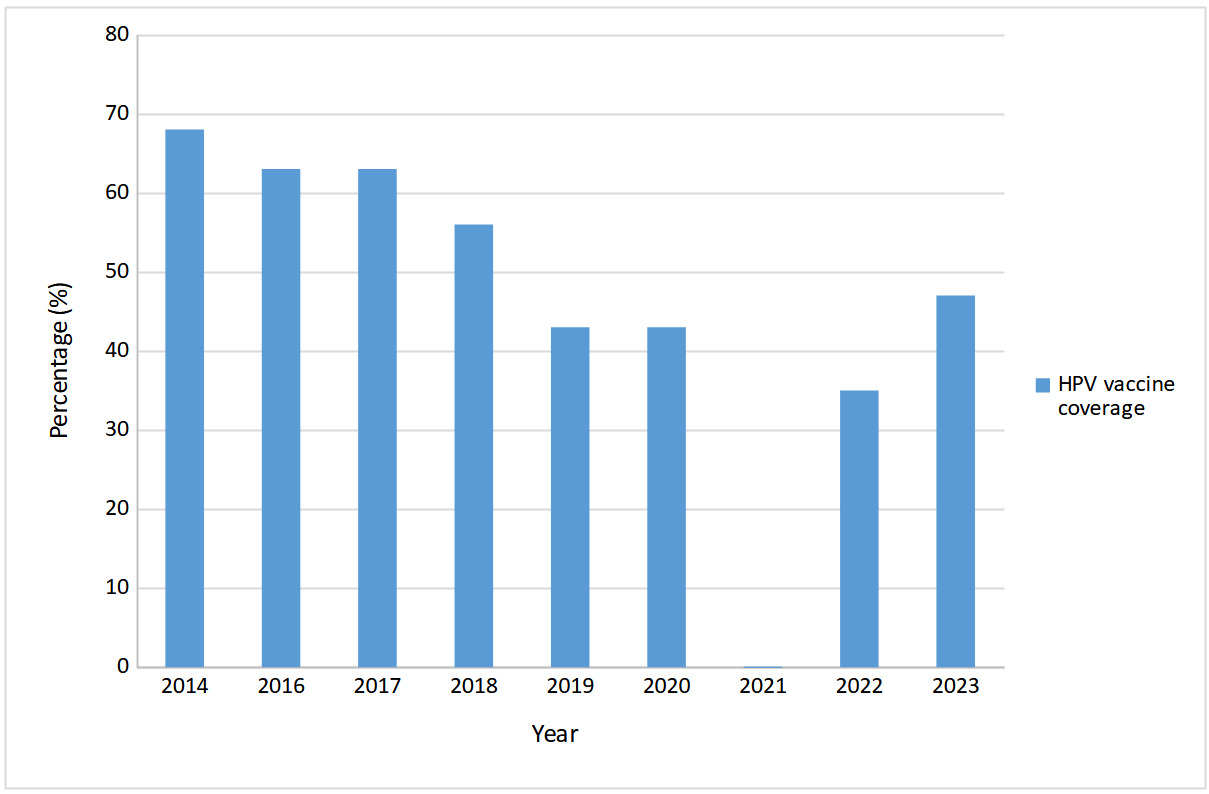
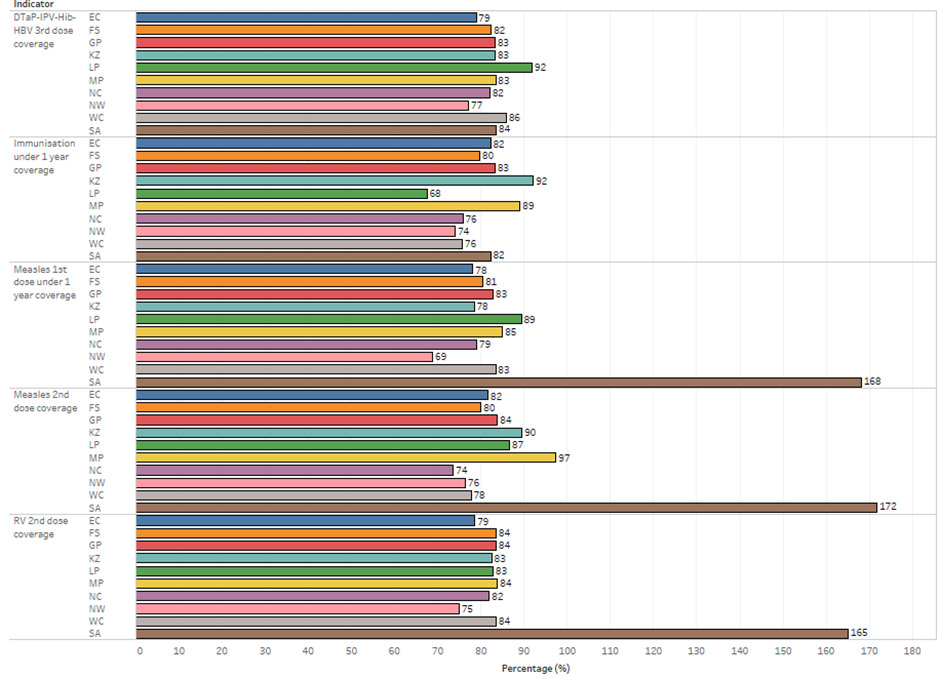
Overall, the evidence underscores the need for innovative interventions and strategies, including enhanced education about cancers and surveillance across all population groups. One of the most important interventions is vaccination against human papillomavirus (HPV), which has the potential to advance eradication of cervical cancer in women. Figure 4 shows the dramatic negative impact on HPV vaccine coverage during the COVID-19 pandemic, as reported by WHO.14 Coverage has not yet recovered to pre-pandemic levels. As per the Global Strategy for Cervical Cancer Elimination,3 each country should introduce HPV in the national immunisation schedule by 2030 and meet the target of 90% of girls fully vaccinated with HPV vaccine by age 15. A WHO dashboard contains data on the status of HPV vaccine introduction in WHO member states.14
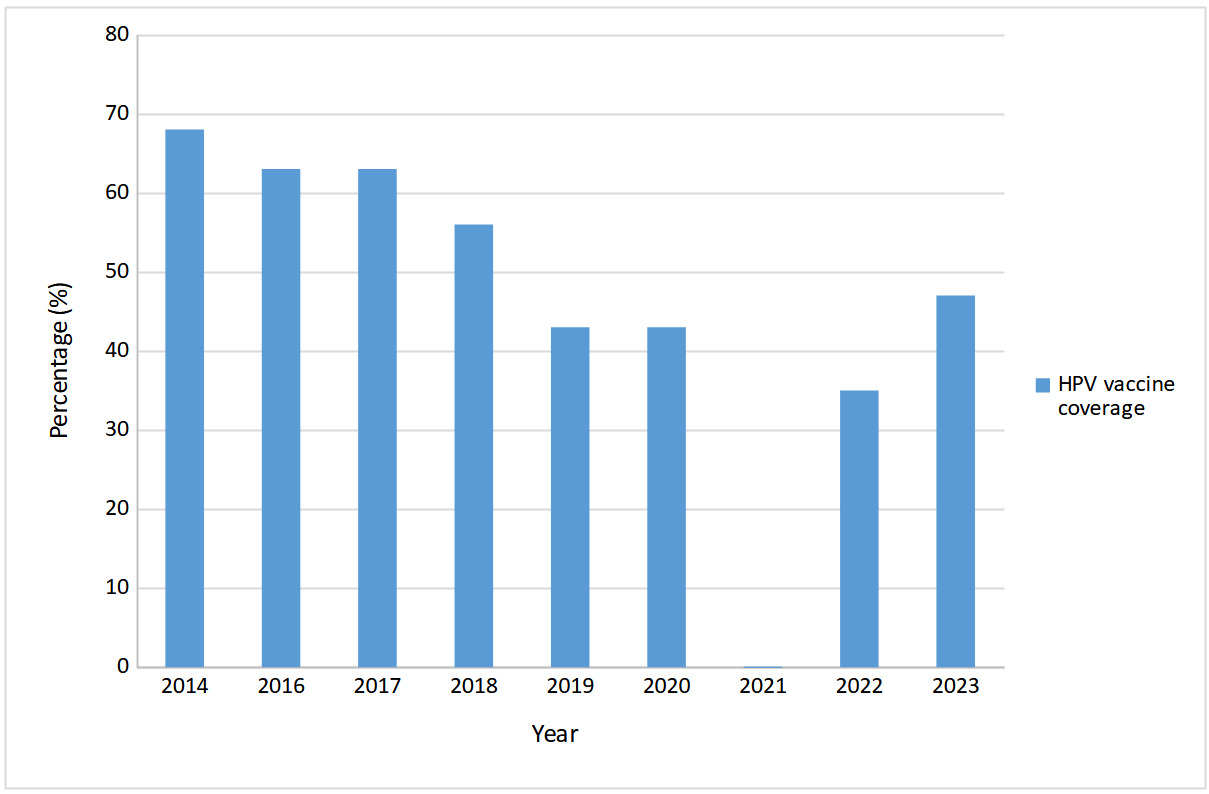
Figure 4.HPV vaccine programme coverage in females in South Africa, 2014-2022
*Data for 2021 were missing.
Source: WHO HPV Dashboard, 2024.14
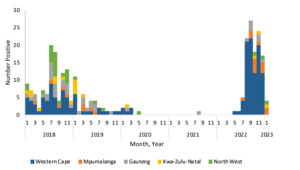
Figure 5 shows a similar impact on cervical screening coverage, with modest recovery post-pandemic, presumably due to diagnostic service rearrangement following the brief suspension of cancer screening services.15

Figure 5.Cervical cancer screening coverage rates among women 30 years and older, 2015-2022
Lung cancer
The Tobacco Products and Electronic Delivery Systems Control Bill (Bill 33 of 2022) has been tabled but will need to be revived by the new Parliament.17 Van Eeden et al. have pointed out that there are no official lung cancer screening programmes in South Africa.18 These authors also note that improved thoracic surgery, systemic therapies, pathological research, and lung tumour radiation are mostly available in the private sector in South Africa. Public sector patients “have limited access to treatment, and those who do are often managed with the use of simpler techniques and very basic therapies.”18(p27) Qualitative data reveal that KwaZulu-Natal public sector lung cancer screening, early diagnosis, treatment, and palliative care are inadequate.19 However, statistics for sector-specific treatment results are hard to find. In 2022, GLOBOCAN reported that lung cancer was the second most diagnosed new cancer in men (11.6%) and the fourth in women (5.8%). Lung cancer was diagnosed in 9 446 South African men and women in 2022. In the same year, 8 672 died from lung cancer.8
Breast cancer
Breast cancer data show large public-private care discrepancies. Breast cancer incidence has increased, but South Africa has a lower incidence and higher death rate than high-income countries due to lower screening rates and poorer access to care.20 In addition, poorer outcomes may be linked to a higher proportion of triple-negative breast cancer in patients who are black African. Women in South Africa tend to present with late-stage disease, reflecting poor screening and access to diagnosis and care.
Health and socio-economic indicators: burden of disease and beyond
As in previous editions of the Review, the next sections of this paper aim to provide a repository of provincial and national data describing the current status of the South African health system (socio-demographic indicators and determinants, health-status indicators, and health-service indicators). The paper can also, at least in relation to the public sector, be read together with the most recent edition of the District Health Barometer (DHB), which has been published after a short hiatus.21 Like the DHB, the Review aims to highlight inequities in health outcomes and health-resource allocation and delivery. Cancer is by no means immune to the effects of those inequities.
Data sources
The key new or updated sources relied upon, at both an international and a national level, are shown in Box 1. Specific references and the current indicator definitions are provided in the data tables. Many of the indicators are normalised using population denominators.
The 2022 Census conducted by Stats SA is a cornerstone for policy development and resource allocation across the nation. While the census data is intended to provide an accurate snapshot of the country’s demographics, concerns have been raised regarding their validity and accuracy, with some stakeholders questioning the reliability of the published data.22 In response, Stats SA has strongly refuted these claims, defending the robustness of their methodologies and the accuracy of the results.23 Despite this, the debate highlights the critical importance of data integrity in shaping informed decision-making.
Box 1.Key new or updated health data sources, 2023
| International |
South African |
- World Health Statistics 202324
- World Malaria Report 202325
- The Fordham Disability Data Report 202326
- Global Tuberculosis Report 202327
- State of World’s Children 202328
- UNAIDS Update 202329
- Immunization update 202330
- WHO Global report on trends in prevalence of tobacco use 2000-203031
- Human Development Report 2023/2432
- Global Cancer Observatory8
|
- Census 202233
- Stats SA General Household Survey (GHS) 202234
- South African National HIV Prevalence, Incidence, Behaviour and Communication Survey, 2022 (SABSSM VI)35
- The 2022 Antenatal HIV Sentinel Survey: key findings36
- Saving Mothers 202137 and 202238
- Stats SA Mortality and Causes of Death 201939
- Stats SA Road Transport Accident Deaths40
- Stats SA Labour Force Surveys up to the 4th quarter of 202341
- Stats SA Recorded Live Births 202242
- National Blue Drop Report 202343
- National Green Drop Watch Report 202344
- National Cancer Registry11
- National Treasury Health Expenditure data45
- Personnel Administration System (PERSAL)46
- South African Community Epidemiology Network on Drug Use (SACENDU)47
- Council for Medical Schemes Industry Report 202248
|
Demographic indicators
Population dynamics influence the implementation of strategies for achieving sustainable development goals within a country. The COVID-19 pandemic, which lowered the country’s life expectancy in 2021 and had an influence on mortality and migration, began four years ago. The COVID-19 pandemic caused a demographic shift in death and morbidity, notably among older people. However, it is unknown whether the pandemic had any long-term consequences on demography, such as changes in age structure or fertility.49 Every year, Stats SA produces mid-year population estimates (MYPEs). However, due to the release of Census 2022 findings in 2023, no MYPEs were issued for 2023.
According to the Census 2022 statistics, South Africa’s total population has climbed to 62 million individuals from 51 million in 2011. The findings also show that the populations of the Western Cape, Gauteng, North West, and Northern Cape have increased due to internal migration, with more individuals moving into these provinces rather than out. By contrast, Limpopo, the Eastern Cape, and KwaZulu-Natal have greater out-migration rates. These figures have significance for the National Treasury’s equitable share allocation mechanism, which determines the provincial allocation of budget for health programmes from the fiscus. The basic demographic figures are provided in Table 1.
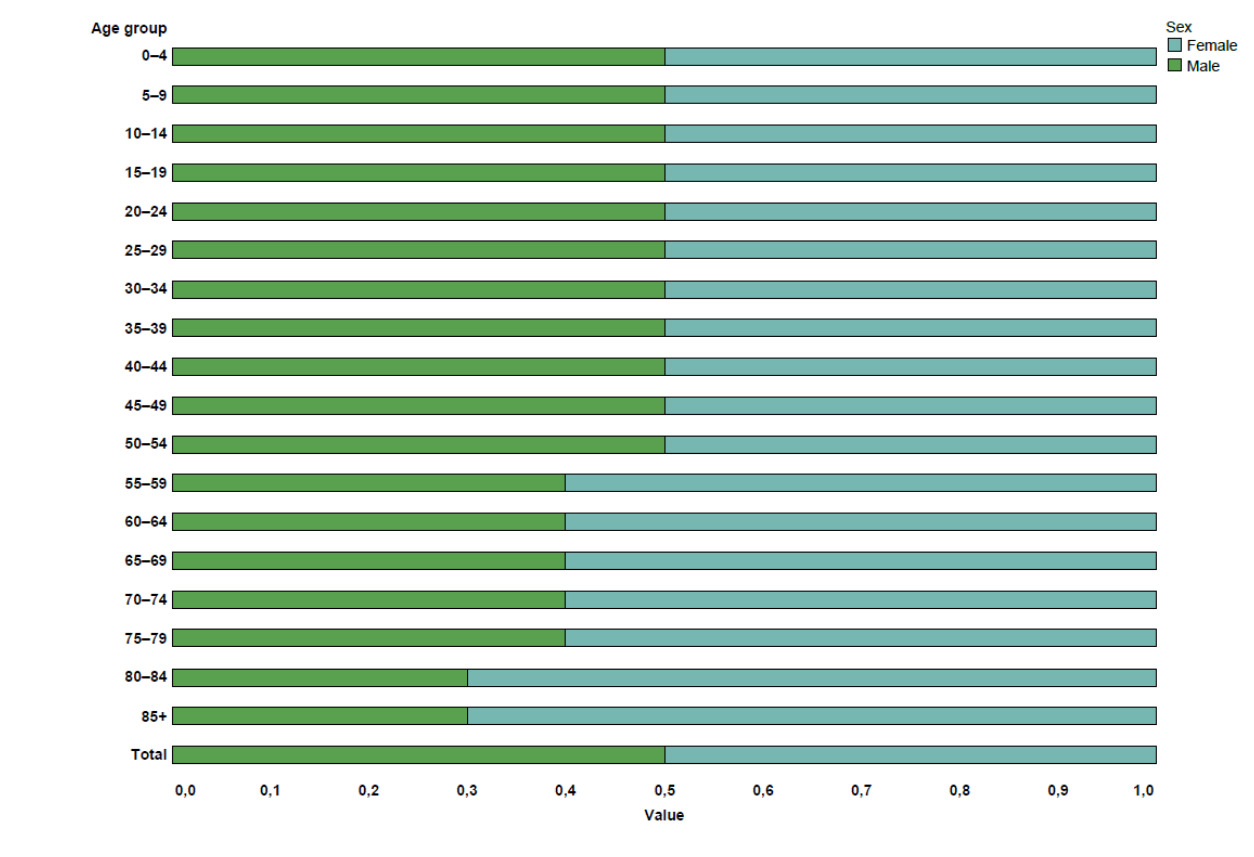
Figure 6 depicts South Africa’s ageing population. An elderly population is also more likely to develop non-communicable diseases. South Africa has a higher proportion of females than males, with the gap becoming apparent between the ages of 54 and 59. Between 2013 and 2021, the adolescent fertility rate was 40.7 per 1 000 girls aged 15 to 19.24 South Africa’s median age is 28 years, and it is predicted that 61.2% of the population is aged 15 to 34.33 As a result, South Africa could profit from capitalising on the economic benefits of its age structure by boosting the proportion of working-age adults compared to young dependents.
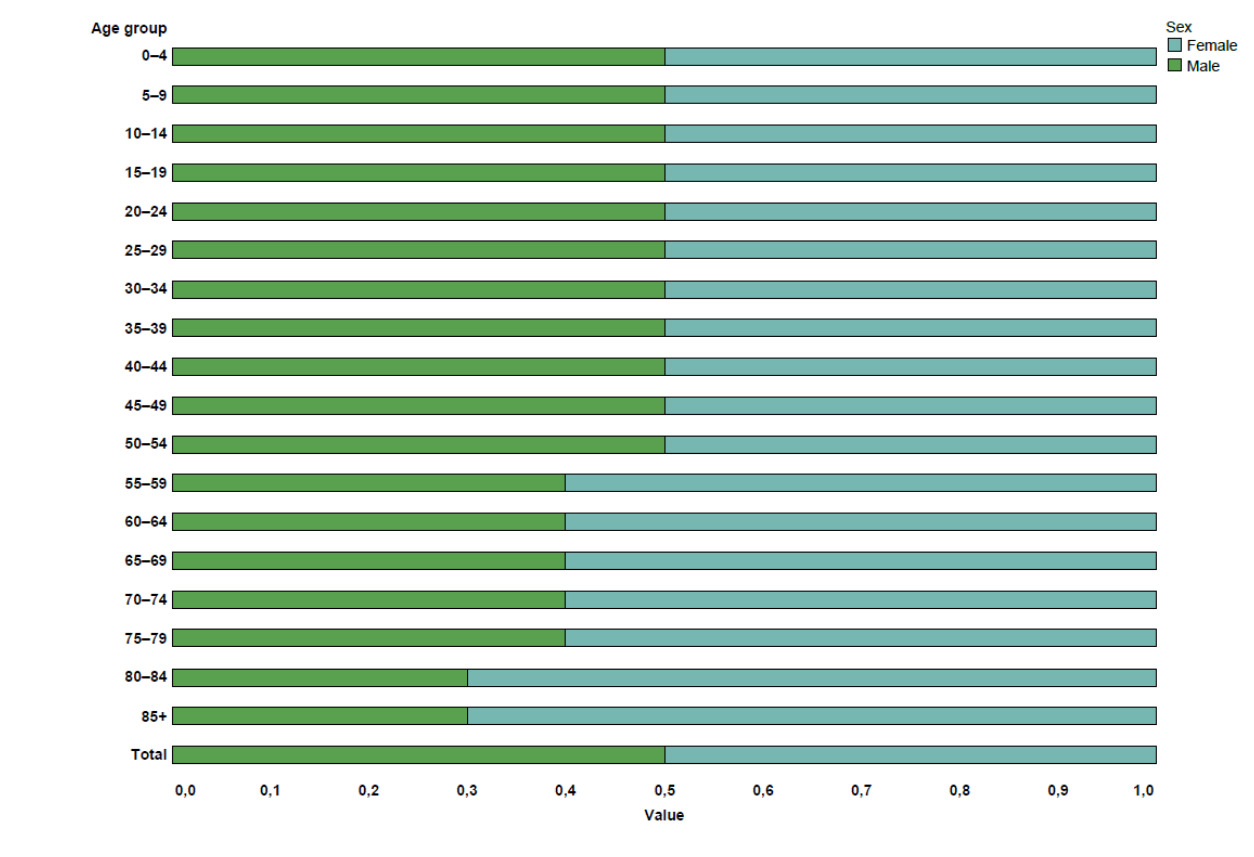
Figure 6.The distribution of females and males by age group in South Africa
Source: Census 2022, Statistics South Africa.33
Table 2 contains revised estimates for uninsured people by province and district, which are key denominators for a variety of health measures.
Table 1.Demographic indicators by province
| Indicator |
Period |
Sex|Age|Series|Cat |
SA |
EC |
FS |
GP |
KZ |
LP |
MP |
NC |
NW |
WC |
Ref |
Adolescent fertility rate (per 1000 girls aged
15–19 years) |
2013-2021 |
female 15-19 years WHO |
40,7 |
|
|
|
|
|
|
|
|
|
a |
| Age dependency ratio |
2022 |
Census |
48,8 |
60,0 |
50,7 |
38,9 |
50,5 |
62,7 |
50,6 |
52,5 |
52,7 |
42,2 |
b |
| Area (square km) |
2018 |
Census 2018 boundaries |
1 220 813 |
168 966 |
129 825 |
18 178 |
94 361 |
125 754 |
76 495 |
372 889 |
104 882 |
129 462 |
c |
| Area as a % of total area of South Africa |
2018 |
Census 2018 boundaries |
100 |
13,8 |
10,6 |
1,5 |
7,7 |
10,3 |
6,3 |
30,5 |
8,6 |
10,6 |
c |
| Average household size |
2022 |
Census |
3,5 |
3,9 |
3,5 |
2,8 |
4,4 |
3,6 |
3,6 |
4,1 |
3,3 |
3,3 |
b |
| Live birth occurrences registered |
2022 |
vital registration total |
998 362 |
113 085 |
46 797 |
231 816 |
219 806 |
124 065 |
85 216 |
24 674 |
58 732 |
94 171 |
d |
| Population |
2022 |
both sexes all ages Census |
62 027 503 |
7 230 204 |
2 964 412 |
15 099 422 |
12 423 907 |
6 572 721 |
5 143 324 |
1 355 945 |
3 804 548 |
7 433 020 |
b |
| both sexes all ages Stats SA 2019-30 FinYr total |
61 220 537 |
6 551 888 |
3 020 662 |
16 271 412 |
11 847 316 |
6 004 534 |
4 815 440 |
4 242 620 |
1 283 976 |
7 182 690 |
e |
| female all ages Census |
31 947 531 |
|
|
|
|
|
|
|
|
|
b |
| male all ages Census |
30 076 814 |
|
|
|
|
|
|
|
|
|
b |
| 2022/23 |
both sexes all ages DHIS 2000-2030 FinYr total |
61 402 320 |
6 711 415 |
2 920 478 |
16 362 152 |
11 683 165 |
6 124 442 |
4 815 060 |
1 310 808 |
4 231 279 |
7 243 521 |
f |
| 2023 |
both sexes all ages Stats SA |
62 078 055 |
6 558 165 |
3 036 315 |
16 664 257 |
11 953 445 |
6 051 055 |
4 886 200 |
4 308 772 |
1 298 509 |
7 321 339 |
e |
| 2023/24 |
both sexes all ages DHIS 2000-2030 FinYr total |
62 197 960 |
6 709 060 |
2 930 982 |
16 723 636 |
11 801 471 |
6 165 877 |
4 880 047 |
1 324 275 |
4 293 016 |
7 369 596 |
f |
| Population % by province |
2022 |
both sexes all ages Census |
100 |
11,7 |
4,8 |
24,3 |
20,0 |
10,6 |
8,3 |
2,2 |
6,1 |
12,0 |
b |
| Population % composition |
2022 |
female Census |
51,5 |
52,6 |
52,5 |
49,5 |
52,4 |
52,8 |
52,0 |
51,8 |
50,5 |
51,5 |
b |
| male Census |
48,5 |
47,4 |
47,5 |
50,5 |
47,6 |
47,2 |
48,0 |
48,2 |
49,5 |
48,5 |
b |
| Population under 1 year |
2022/23 |
DHIS |
1 135 768 |
131 213 |
50 358 |
261 993 |
254 035 |
125 299 |
95 085 |
25 279 |
80 653 |
111 853 |
g |
| Public sector dependent (uninsured) population |
2022 |
both sexes all ages GHS |
51 029 403 |
5 968 962 |
2 497 977 |
12 524 688 |
10 257 571 |
5 412 651 |
4 239 006 |
1 103 263 |
3 617 554 |
5 394 682 |
h |
References notes
a World Health Statistics 2023.24
b Census 2022.33
c Census 2022 Provinces.50
d Stats SA Live Births 2022.42
e Pop Est 2019-30.51
f webDHIS Pop Est 2000-30.16
g webDHIS.16
h Stats SA GHS 2022.34
Definitions
• Area (square km) [km2]: Land area covered by geographic entity.
• Population [Number]: Total number of people. Projected population figures are based on various projection models attempting to quantify the expected effects of HIV and AIDS on population growth.
• Adolescent fertility rate (per 1 000 girls aged 15-19 years): Annual number of births to women aged 15-19 years per 1 000 women in that age group. Also referred to as the age-specific fertility rate for women aged 15-19 years.
• Age dependency ratio [Number]: The ratio of the combined child population (0-14 years) and the aged population (65 years and over) - persons in the dependent ages - to every 100 people of the intermediate age population (15-65 years) - economically active ages.
• Ageing index [Number]: Ratio of the number of people 65+ to the number under 15 years. i.e., a value of 16 means there are 16 people aged 65 and over for every 100 under 15 years of age. Calculated as ([65+/0-14] *100).
• Annual population growth rate [Percentage]: The rate at which the population is increasing or decreasing in a given year expressed as a percentage of the base population size. It takes into consideration all the components of population growth, namely births, deaths and migration.
• Area as a % of total area of South Africa [Percentage]: Area of province divided by total area of country (South Africa).
• Average household size [Number]: Average number of people living in each household where household is defined as a person, or a group of persons, who occupy a common dwelling (or part of it) for at least four days a week and who provide themselves jointly with food and other essentials for living. In other words, they live together as a unit. People who occupy the same dwelling, but who do not share food or other essentials, are enumerated as separate households.
• Live birth occurrences registered: The number of live birth occurrences registered.
• Population % by province [Percentage]: Proportion of South African population in each province (calculated from population per province and population for whole of South Africa).
• Population % composition [Percentage]: Percentage of the population by various categories.
• Population density [people per km2]: The number of people per square kilometre.
• Population under 1 year [Number]: Population under 1 year of age.
• Public sector dependent (uninsured) population [Number]: This is an adjustment of the total population to the number assumed to be dependent on services in the public health sector based on medical scheme (health insurance) coverage. It is calculated by subtracting the number of people with medical scheme cover (determined from medical scheme membership reports, or surveys indicating percentage of population on medical schemes) from the total population.
• Total fertility rate [Number]: The average number of children that a woman gives birth to in her lifetime, assuming that the prevailing rates remain unchanged.
Table 2.Population estimates, modelled estimates for medical schemes coverage and uninsured population, national, provincial and district, 2020-202452
|
|
Total Population (DHIS Pop Est 2000-30) |
Med schemes
coverage (Insight
Actuaries model
2019) |
Uninsured Calculated |
|
2020 |
2021 |
2022 |
2023 |
2024 |
2018 |
2020 |
2021 |
2022 |
2023 |
2024 |
| Country |
ZA |
59 797 656 |
60 604 086 |
61 402 320 |
62 197 960 |
62 997 254 |
15,4 |
50 588 817 |
51 271 057 |
51 946 363 |
52 619 474 |
53 295 677 |
| Province |
EC |
6 713 318 |
6 714 789 |
6 711 415 |
6 709 060 |
6 707 731 |
9,8 |
6 055 413 |
6 056 740 |
6 053 696 |
6 051 572 |
6 050 373 |
| FS |
2 900 278 |
2 910 130 |
2 920 478 |
2 930 982 |
2 941 782 |
13,5 |
2 508 740 |
2 517 262 |
2 526 213 |
2 535 299 |
2 544 641 |
| GP |
15 635 579 |
15 997 809 |
16 362 152 |
16 723 636 |
17 085 122 |
24,6 |
11 789 227 |
12 062 348 |
12 337 063 |
12 609 622 |
12 882 182 |
| KZN |
11 441 785 |
11 563 182 |
11 683 165 |
11 801 471 |
11 919 341 |
11,2 |
10 160 305 |
10 268 106 |
10 374 651 |
10 479 706 |
10 584 375 |
| LP |
6 039 032 |
6 084 467 |
6 124 442 |
6 165 877 |
6 208 983 |
7,2 |
5 604 222 |
5 646 385 |
5 683 482 |
5 721 934 |
5 761 936 |
| MP |
4 680 103 |
4 748 543 |
4 815 060 |
4 880 047 |
4 944 155 |
12,5 |
4 095 090 |
4 154 975 |
4 213 178 |
4 270 041 |
4 326 136 |
| NC |
1 282 813 |
1 297 034 |
1 310 808 |
1 324 275 |
1 337 691 |
15,1 |
1 089 108 |
1 101 182 |
1 112 876 |
1 124 309 |
1 135 700 |
| NW |
4 107 283 |
4 169 094 |
4 231 279 |
4 293 016 |
4 354 742 |
11,9 |
3 618 516 |
3 672 972 |
3 727 757 |
3 782 147 |
3 836 528 |
| WC |
6 997 465 |
7 119 038 |
7 243 521 |
7 369 596 |
7 497 707 |
20,1 |
5 590 975 |
5 688 111 |
5 787 573 |
5 888 307 |
5 990 668 |
| District |
BUF |
798 388 |
796 759 |
794 314 |
791 614 |
788 728 |
22,4 |
619 549 |
618 285 |
616 388 |
614 292 |
612 053 |
| CPT |
4 598 783 |
4 686 530 |
4 776 492 |
4 867 548 |
4 959 961 |
22,2 |
3 577 853 |
3 646 120 |
3 716 111 |
3 786 952 |
3 858 850 |
| DC1 |
463 390 |
471 043 |
478 958 |
487 115 |
495 538 |
17,3 |
383 224 |
389 553 |
396 098 |
402 844 |
409 810 |
| DC2 |
942 232 |
958 398 |
974 747 |
991 117 |
1 007 633 |
16,4 |
787 706 |
801 221 |
814 888 |
828 574 |
842 381 |
| DC3 |
299 764 |
305 203 |
310 662 |
316 173 |
321 761 |
16,4 |
250 603 |
255 150 |
259 713 |
264 321 |
268 992 |
| DC4 |
618 954 |
623 516 |
628 217 |
633 013 |
637 944 |
16,5 |
516 827 |
520 636 |
524 561 |
528 566 |
532 683 |
| DC5 |
74 342 |
74 348 |
74 445 |
74 630 |
74 870 |
12,5 |
65 049 |
65 055 |
65 139 |
65 301 |
65 511 |
| DC6 |
114 035 |
114 077 |
114 245 |
114 367 |
114 491 |
17,5 |
94 079 |
94 114 |
94 252 |
94 353 |
94 455 |
| DC7 |
206 326 |
208 167 |
209 912 |
211 609 |
213 309 |
13,1 |
179 297 |
180 897 |
182 414 |
183 888 |
185 366 |
| DC8 |
278 104 |
282 362 |
286 400 |
290 296 |
294 142 |
15,8 |
234 164 |
237 749 |
241 149 |
244 429 |
247 668 |
| DC9 |
414 190 |
417 771 |
421 181 |
424 540 |
427 897 |
15,7 |
349 162 |
352 181 |
355 056 |
357 887 |
360 717 |
| DC10 |
480 810 |
483 024 |
484 665 |
486 523 |
488 581 |
8,8 |
438 499 |
440 518 |
442 014 |
443 709 |
445 586 |
| DC12 |
795 781 |
787 417 |
778 884 |
770 438 |
762 037 |
4,3 |
761 562 |
753 558 |
745 392 |
737 309 |
729 269 |
| DC13 |
731 081 |
721 434 |
712 004 |
702 218 |
692 046 |
4,9 |
695 258 |
686 084 |
677 116 |
667 809 |
658 136 |
| DC14 |
342 580 |
340 685 |
338 445 |
336 219 |
334 011 |
5,0 |
325 451 |
323 651 |
321 523 |
319 408 |
317 310 |
| DC15 |
1 524 972 |
1 541 080 |
1 555 812 |
1 571 532 |
1 588 236 |
4,2 |
1 460 923 |
1 476 355 |
1 490 468 |
1 505 528 |
1 521 530 |
| DC16 |
127 071 |
127 119 |
127 251 |
127 471 |
127 766 |
10,5 |
113 729 |
113 772 |
113 890 |
114 087 |
114 351 |
| DC18 |
643 043 |
643 503 |
644 397 |
645 123 |
645 780 |
12,0 |
565 878 |
566 283 |
567 069 |
567 708 |
568 286 |
|
DC19 |
755 842 |
756 396 |
757 178 |
758 118 |
759 199 |
9,2 |
686 305 |
686 808 |
687 518 |
688 371 |
689 353 |
| DC20 |
505 057 |
505 879 |
506 744 |
507 595 |
508 423 |
13,2 |
438 389 |
439 103 |
439 854 |
440 592 |
441 311 |
| DC21 |
816 195 |
827 384 |
838 645 |
850 311 |
862 408 |
7,1 |
758 245 |
768 640 |
779 101 |
789 939 |
801 177 |
| DC22 |
1 137 023 |
1 150 285 |
1 163 352 |
1 177 092 |
1 191 603 |
11,0 |
1 011 950 |
1 023 754 |
1 035 383 |
1 047 612 |
1 060 527 |
| DC23 |
706 771 |
708 994 |
711 516 |
714 070 |
716 629 |
6,4 |
661 538 |
663 618 |
665 979 |
668 370 |
670 765 |
| DC24 |
563 568 |
569 454 |
575 760 |
582 409 |
589 451 |
5,4 |
533 135 |
538 703 |
544 669 |
550 959 |
557 621 |
| DC25 |
565 495 |
572 008 |
577 873 |
583 415 |
588 740 |
7,4 |
523 648 |
529 679 |
535 110 |
540 242 |
545 173 |
| DC26 |
863 111 |
867 237 |
872 128 |
877 196 |
882 407 |
5,2 |
818 229 |
822 141 |
826 777 |
831 582 |
836 522 |
| DC27 |
676 068 |
680 655 |
685 592 |
690 192 |
694 486 |
5,0 |
642 265 |
646 622 |
651 312 |
655 682 |
659 762 |
| DC28 |
964 828 |
969 742 |
975 004 |
980 188 |
985 306 |
8,7 |
880 888 |
885 374 |
890 179 |
894 912 |
899 584 |
| DC29 |
680 361 |
688 960 |
696 590 |
703 372 |
709 399 |
8,6 |
621 850 |
629 709 |
636 683 |
642 882 |
648 391 |
| DC30 |
1 240 644 |
1 262 612 |
1 283 719 |
1 304 284 |
1 324 497 |
13,1 |
1 078 120 |
1 097 210 |
1 115 552 |
1 133 423 |
1 150 988 |
| DC31 |
1 613 205 |
1 645 648 |
1 677 409 |
1 708 843 |
1 740 152 |
14,8 |
1 374 451 |
1 402 092 |
1 429 152 |
1 455 934 |
1 482 610 |
| DC32 |
1 826 254 |
1 840 283 |
1 853 932 |
1 866 920 |
1 879 506 |
10,2 |
1 639 976 |
1 652 574 |
1 664 831 |
1 676 494 |
1 687 796 |
| DC33 |
1 218 016 |
1 226 939 |
1 234 474 |
1 241 931 |
1 249 341 |
6,8 |
1 135 191 |
1 143 507 |
1 150 530 |
1 157 480 |
1 164 386 |
| DC34 |
1 474 045 |
1 488 161 |
1 501 251 |
1 514 770 |
1 528 782 |
6,6 |
1 376 758 |
1 389 942 |
1 402 168 |
1 414 795 |
1 427 882 |
| DC35 |
1 349 214 |
1 353 845 |
1 357 666 |
1 361 654 |
1 365 871 |
8,3 |
1 237 229 |
1 241 476 |
1 244 980 |
1 248 637 |
1 252 504 |
| DC36 |
769 853 |
776 172 |
781 264 |
786 231 |
791 149 |
9,1 |
699 796 |
705 540 |
710 169 |
714 684 |
719 154 |
| DC37 |
1 929 057 |
1 972 917 |
2 015 765 |
2 058 230 |
2 100 644 |
14,0 |
1 658 989 |
1 696 709 |
1 733 558 |
1 770 078 |
1 806 554 |
| DC38 |
906 601 |
910 841 |
916 394 |
922 575 |
929 280 |
9,7 |
818 661 |
822 489 |
827 504 |
833 085 |
839 140 |
| DC39 |
471 910 |
473 588 |
475 637 |
477 280 |
478 586 |
7,3 |
437 461 |
439 016 |
440 915 |
442 439 |
443 649 |
| DC40 |
799 715 |
811 748 |
823 483 |
834 931 |
846 232 |
12,8 |
697 351 |
707 844 |
718 077 |
728 060 |
737 914 |
| DC42 |
963 811 |
966 230 |
968 999 |
972 188 |
975 815 |
20,8 |
763 338 |
765 254 |
767 447 |
769 973 |
772 845 |
| DC43 |
506 908 |
510 113 |
513 778 |
517 618 |
521 648 |
5,6 |
478 521 |
481 547 |
485 006 |
488 631 |
492 436 |
| DC44 |
828 210 |
830 067 |
831 112 |
832 500 |
834 220 |
3,8 |
796 738 |
798 524 |
799 530 |
800 865 |
802 520 |
| DC45 |
270 158 |
274 657 |
279 070 |
283 463 |
287 852 |
13,9 |
232 606 |
236 480 |
240 279 |
244 062 |
247 841 |
| DC47 |
1 227 904 |
1 239 350 |
1 249 787 |
1 261 291 |
1 273 840 |
5,6 |
1 159 141 |
1 169 946 |
1 179 799 |
1 190 659 |
1 202 505 |
| DC48 |
956 893 |
969 545 |
982 753 |
996 636 |
1 011 253 |
24,1 |
726 282 |
735 885 |
745 910 |
756 447 |
767 541 |
| EKU |
3 996 528 |
4 080 699 |
4 165 110 |
4 250 640 |
4 337 642 |
23,8 |
3 045 354 |
3 109 493 |
3 173 814 |
3 238 988 |
3 305 283 |
| ETH |
3 961 457 |
4 018 350 |
4 072 927 |
4 125 608 |
4 177 264 |
18,9 |
3 212 742 |
3 258 882 |
3 303 144 |
3 345 868 |
3 387 761 |
| JHB |
5 951 077 |
6 121 322 |
6 295 072 |
6 465 812 |
6 635 068 |
22,2 |
4 629 938 |
4 762 389 |
4 897 566 |
5 030 402 |
5 162 083 |
|
MAN |
869 265 |
877 233 |
884 908 |
892 675 |
900 614 |
20,0 |
695 412 |
701 786 |
707 926 |
714 140 |
720 491 |
| NMA |
1 211 496 |
1 214 323 |
1 216 179 |
1 218 016 |
1 219 872 |
20,4 |
964 351 |
966 601 |
968 078 |
969 541 |
971 018 |
| TSH |
3 767 270 |
3 860 013 |
3 950 218 |
4 038 360 |
4 125 344 |
30,6 |
2 614 485 |
2 678 849 |
2 741 451 |
2 802 622 |
2 862 989 |
Socio-economic and environmental risk factors
The social pathways of health reflect conditions in which populations navigate life on a day-to-day basis, such as employment status, education, air pollution and climate change.32 All of these factors have an impact on people’s livelihoods and health status.
Human development and inequality
The United Nations Development Programme’s 2023/2024 Human Development Report investigates impediments that polarise the world’s inequities in health, education, gender, and income. According to this report, South Africa is ranked 105 out of 193 countries, in terms of the Human Development Index (HDI).29 The HDI for South Africa shows improvements between 2000 (0.695) and 2019 (0.727), but then begins to decline in later years, particularly during the COVID-19 pandemic, and has continued to decline.
In understanding global poverty, the Human Development Report Office (HDRO) and the Oxford Poverty and Human Development Initiative produce the Multidimensional Poverty Index (MPI) for 110 developing countries, including South Africa.53 The MPI is based on the latest household-level survey data and considers various dimensions of poverty, such as nutrition, years of schooling, school attendance, child mortality, cooking fuel, housing, sanitation, electricity, drinking water, and assets. The MPI value represents the proportion of the population that is multi-dimensionally poor, adjusted by the intensity of their deprivations.
Social inequality and unemployment
For South Africa, the MPI value is 0.025. Approximately 0.9% of South Africans are in severe multidimensional poverty, 12.2% are vulnerable to multidimensional poverty, and 20.5% are below the income poverty line.30
South Africa continues to struggle with social inequality in a constrained economy and limited fiscal space. Table 3 shows that, by the conclusion of the fourth quarter of 2023, South Africa had about 7.9 million unemployed people. However, the economy contracted by 0.63%, following a 1.2% gain in the fourth quarter of 2022.41
Air pollution and health
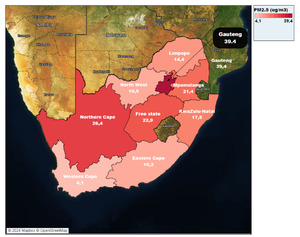
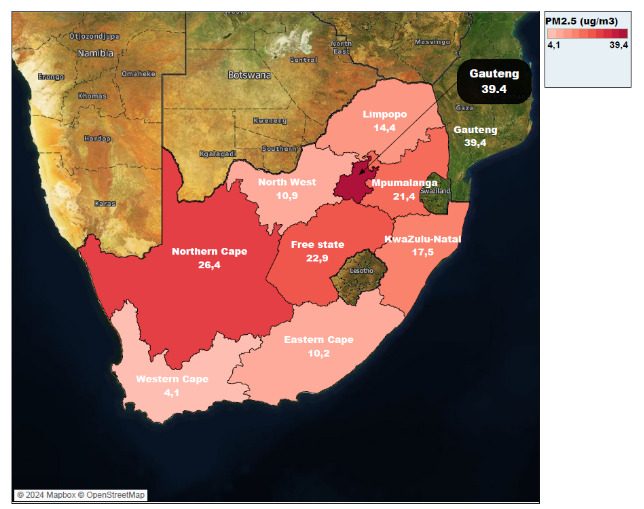
It is reported that one in every eight deaths globally is due to air pollution exposure, that is, more than human immunodeficiency virus (HIV), tuberculosis (TB) and malaria combined.54 According to the World Health Statistics, 8.8% of South Africans rely on clean fuels to use for cooking, heating and lighting, despite the fact that clean fuels such as solar and biogas have been shown to meet the guidelines for indoor pollution.24,55 Aerodynamic pollutants with a diameter of less than 2.5μm, referred to as particulate matter (PM2.5), can damage the respiratory tract. Figure 7 demonstrates that Gauteng and the Northern Cape have the highest amounts of PM2.5. In the Northern Cape, this can be related to the dispersion of mining dust or sand from the Namib Desert, as well as salt from the Atlantic Ocean. In Gauteng, this is attributed to pollution from vehicles and industry.56
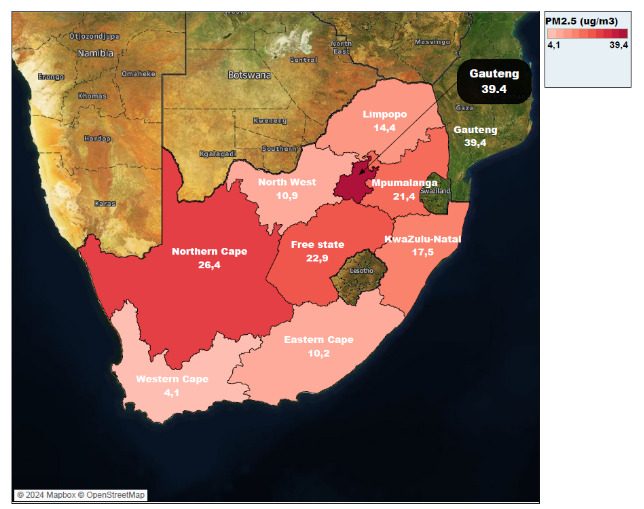
Figure 7.Concentration of PM2.5 levels by province, 2021
Monitoring air pollution
Monitoring air pollution, specifically PM2.5 levels, is critical for tracking progress towards the Sustainable Development Goals (SDG indicator 3.9.1). The WHO recommends limiting yearly PM2.5 concentrations to 5 μg/m3 (annual average) and 15 μg/m3 (24-hour average) for more than 3-4 days per year. According to IQAir, a Swiss business, most countries are failing to meet the WHO health guideline for PM2.5, based on data from at least 30 000 monitoring stations worldwide.58 Figure 8 illustrates that PM2.5 monitoring in South Africa is sparsely dispersed, with data accessible mostly in industrial and mining cities with high PM2.5 concentrations. As such, air pollution research could focus on understanding the spatial heterogeneities of air pollution exposure that may occur in South Africa. Air pollution is a public health hazard, and the actions and instruments to combat it are unevenly distributed around the world. The WHO defines quality of life as the population’s physical health and social relationships with the environment, and there are major differences in how air pollution impacts them.59

Figure 8.Concentrations of PM2.5 levels in South Africa by year and city
Source: WHO Database Ambient Air Quality, 2021.32
Adebayo et al. have pointed out that air pollution, in particular PM2.5, is associated with the mortality of people with comorbidities.35 Burnett et al. argue that exposure to PM2.5 may be associated with additional causes of death than the usual top five considered by the Global Burden of Diseases.36 According to the Air Quality Life Index (AQLI) report, if PM2.5 pollution is permanently eliminated to meet the WHO guidelines, it would result in an increase in the average human life expectancy by 2.3 years.57 The impact of PM2.5 on global life expectancy is comparable to that of smoking elimination, over three times greater than that of alcohol use and unsafe water, more than five times larger than transport injuries like car accidents, and over seven times greater than that of HIV/AIDS.34
Water quality and public health
The Department of Water and Sanitation’s Green Drop Watch Report is a crucial initiative to monitor wastewater systems, both at the municipal and provincial levels. The 2023 report highlights that 334 municipal wastewater treatment systems (spread across all provinces) were deemed to be in critical condition in 2022, having received Green Drop scores below 31%.44 Similarly, the Blue Drop Watch Report sheds light on the present state of potable water infrastructure in South Africa.43 Although the Stats SA General Household Survey 2022 results indicate that the majority of the population in South Africa has access to safe drinking water, the Blue Drop Watch Report reveals a concerning reality, where 51% of water systems across the country exhibit poor to bad microbiological water quality. Furthermore, only 16% and 14% of water systems demonstrate excellent and good water quality, respectively. A staggering 71% of water plants fail to meet chemical compliance standards.43 Such findings have significant public health implications, as consumption of contaminated water can increase the risk of waterborne diseases such as cholera. For instance, contamination from the Apies River at the Rooiwal treatment plant led to an outbreak of cholera in the Hammanskraal community in 2023.60
Table 3.Socio-economic indicators by province
| Indicator |
Period |
Sex|Age|Series|Cat |
SA |
EC |
FS |
GP |
KZ |
LP |
MP |
NC |
NW |
WC |
Ref |
| Air pollution level in cities (particulate matter) |
2021 |
AQLI PM2.5 |
21,1 |
10,2 |
22,9 |
39,4 |
17,5 |
14,4 |
21,4 |
26,4 |
10,9 |
4,1 |
a |
| Education level: percentage of population with no schooling |
2022 |
20+ years Census |
6,9 |
7,2 |
5,0 |
3,6 |
8,3 |
14,1 |
11,7 |
6,6 |
7,9 |
2,3 |
b |
| 20+ years GHS |
3,3 |
4,1 |
2,6 |
1,1 |
4,3 |
6,2 |
6,2 |
3,8 |
5,2 |
1,1 |
c |
| Percentage of households by type of housing |
2022 |
Census formal |
88,5 |
83,6 |
88,5 |
88,5 |
86,8 |
94,7 |
92,2 |
85,6 |
88,0 |
88,0 |
b |
| Census informal |
8,1 |
4,4 |
9,7 |
11,0 |
5,0 |
2,7 |
5,8 |
12,1 |
10,8 |
11,1 |
b |
| Census other |
0,3 |
0,3 |
0,6 |
0,3 |
0,3 |
0,4 |
0,2 |
0,6 |
0,5 |
0,3 |
b |
| Census traditional |
3,1 |
11,7 |
1,2 |
0,3 |
80,0 |
2,2 |
1,8 |
1,4 |
0,7 |
0,7 |
b |
| GHS Formal |
83,2 |
75,3 |
84,9 |
80,7 |
82,8 |
95,9 |
90,7 |
83,6 |
79,3 |
83,0 |
c |
| GHS Informal |
12,3 |
5,3 |
13,4 |
18,7 |
5,2 |
3,1 |
7,0 |
15,3 |
20,5 |
16,7 |
c |
| GHS Other |
0,3 |
0,5 |
0,1 |
0,6 |
0,1 |
0,0 |
0,0 |
0,6 |
0,0 |
0,2 |
c |
| GHS Traditional |
4,3 |
19,0 |
1,7 |
0,0 |
12,0 |
1,0 |
2,3 |
0,5 |
0,2 |
0,1 |
c |
| Percentage of households using electricity for cooking |
2022 |
both sexes GHS |
76,5 |
77,1 |
86,2 |
76,2 |
82,0 |
63,5 |
74,3 |
78,8 |
76,6 |
75,7 |
c |
| Census |
64,9 |
65,0 |
78,6 |
62,7 |
71,9 |
49,3 |
66,6 |
72,0 |
69,7 |
63,9 |
b |
| Percentage of households using electricity for lighting |
2022 |
Census |
94,7 |
94,5 |
94,6 |
93,2 |
96,7 |
95,5 |
93,7 |
92,5 |
93,9 |
96,5 |
b |
| Percentage of households with access to improved sanitation |
2022 |
GHS |
83,2 |
90,0 |
87,4 |
90,5 |
81,2 |
63,1 |
63,8 |
83,9 |
72,7 |
95,9 |
c |
| Percentage of households with no toilet / bucket toilet |
2022 |
both sexes GHS |
1,0 |
2,2 |
1,1 |
0,1 |
0,6 |
1,2 |
1,5 |
6,0 |
1,8 |
0,7 |
c |
| Census |
3,7 |
4,7 |
5,2 |
2,9 |
3,1 |
4,0 |
2,9 |
9,0 |
2,9 |
4,3 |
b |
| Percentage of households with piped water inside dwellings |
2022 |
Census |
59,7 |
49,5 |
49,0 |
75,0 |
51,8 |
31,4 |
47,0 |
54,5 |
43,3 |
85,5 |
b |
| Percentage of households with refuse removal |
2022 |
Census |
66,3 |
53,3 |
63,5 |
85,0 |
57,7 |
32,0 |
51,1 |
64,4 |
53,5 |
88,7 |
b |
| GHS |
62,6 |
41,5 |
72,2 |
84,3 |
51,0 |
24,4 |
41,5 |
62,0 |
51,0 |
89,2 |
c |
| Percentage of households with telephone (telephone in dwelling or cellphone) |
2022 |
Census cellphone |
92,1 |
87,9 |
91,1 |
93,9 |
92,3 |
93,1 |
93,3 |
85,4 |
90,8 |
92,1 |
b |
| GHS |
95,9 |
91,8 |
93,0 |
97,6 |
95,6 |
97,2 |
97,3 |
89,2 |
95,9 |
95,4 |
c |
| Percentage of population with primary reliance on clean fuels |
2021 |
both sexes WHO |
88,0 |
|
|
|
|
|
|
|
|
|
d |
| Unemployment rate (official definition) |
2021 Q4 |
both sexes 15-64 years LFS |
35,3 |
45,0 |
36,7 |
36,6 |
32,4 |
33,9 |
39,7 |
25,0 |
33,8 |
28,0 |
e |
| 2022 Q4 |
both sexes 15-64 years LFS |
32,7 |
42,1 |
22,1 |
34,0 |
31,4 |
31,8 |
36,1 |
22,1 |
37,0 |
22,5 |
f |
| 2023 Q4 |
both sexes 15-64 years LFS |
32,1 |
41,9 |
37,0 |
33,8 |
29,5 |
30,3 |
34,9 |
26,9 |
39,0 |
20,3 |
g |
Reference notes
a AQLI 2023.57
b Census 2022.33
c Stats SA GHS 2022.34
d World Health Statistics 2023.24
e Labour Force Survey Q4 2021.61
f Labour Force Survey Q4 2022.62
g Stats SA QLFS Q4: 2023.41
Definitions
• Air pollution level in cities (particulate matter [PM]) [ug/m3]: Annual mean concentration of particulate matter of less than 2.5 microns of diameter (PM2.5) [ug/m3] (or of less than 10 microns [PM10] if PM2.5 is not available) in cities.
• Education level: percentage of population with no schooling [Percentage]: Percentage of people in a given age group who have received a particular level of education. Data are presented for the percentage of population aged 20 years and above with no schooling. In some cases, the indicator is presented for a different age category depending on what is available in the source.
• Percentage of households by type of housing [Percentage]: Percentage of households that are categorised as formal, informal, traditional or other.
• Percentage of households using electricity for cooking [Percentage]: Percentage of households using electricity as their main energy source for cooking.
• Percentage of households using electricity for lighting [Percentage]: Percentage of households using electricity for lighting.
• Percentage of households with access to improved sanitation [Percentage]: Percentage of households using improved sanitation facilities (including flush to piped sewer system, flush to septic tank, flush/pour flush to pit, flush/pour flush to elsewhere).
• Percentage of households with no toilet / bucket toilet [Percentage]: Percentage of households that have no toilet or were using a bucket toilet.
• Percentage of households with piped water inside dwellings [Percentage]: Percentage of households with piped water inside dwellings.
• Percentage of households with telephone (telephone in dwelling or cell phone) [Percentage]: Percentage of households with a telephone in the dwelling or a cellular telephone.
• Percentage of households with weekly refuse removal [Percentage]: Percentage of households with weekly refuse removal.
• Percentage of population 20 years and older with no schooling [Percentage]: Percentage of population 20 years and older with no schooling.
• Percentage of population with primary reliance on clean fuels [Percentage]: Percentage of population with primary reliance on clean fuels.
• Unemployment rate (official definition) [Percentage]: The official definition of the unemployed is that they are those people within the economically active population (aged 15-65) who did not have a job or business during the 7 days prior to the interview, want to work and are available to work within two weeks of the interview, and have taken active steps to look for work or to start some form of self-employment in the 4 weeks prior to the interview.
Disability
Globally, an increase in the reported number of people with disabilities is linked to an ageing population, particularly in high-income countries.26 Similar trends are expected to be observed in low- and middle-income countries, where the impact of successful treatments for conditions that were previously life threatening has increased life expectancy.63 The Fordham Research Consortium on Disability released a report in 2023 on the availability of disability data and the potential to produce disability disaggregated indicators at national and subnational levels.40 The report showed that data on the inequities experienced by people with disabilities between and within nations is insufficient, with most national statistics offices failing to publish on data disaggregated by disability status. Only one in five of the datasets that were reviewed between 2009 and 2022 had any questions on functional difficulty.26 People with disabilities will continue to be left behind in global agendas unless the prevalence of disability is quantified accurately. Households headed by people with disabilities have been found to have less access to basic services than households headed by people without disabilities.64
According to the Fordham study, 22.4% of persons aged 15 years and older had functional difficulty, with hearing and vision difficulties accounting for 5.4% and 14.4% respectively.26 These estimates are in contrast with the recently reported disability prevalence from the 2022 Census, which was merely 6%.33 Both assessments indicated that the Eastern Cape had the highest prevalence of disability. This is illustrated in Table 4.
Table 4.Disability indicators by province
| Indicator |
Period |
Sex|Age|Series|Cat |
SA |
EC |
FS |
GP |
KZ |
LP |
MP |
NC |
NW |
WC |
Ref |
| Cataract surgery - total |
2022/23 |
both sexes all ages DHIS |
48 971 |
2 069 |
1 943 |
11 249 |
19 831 |
4 463 |
|
619 |
1 215 |
7 582 |
a |
| Cataract surgery rate |
2022/23 |
both sexes all ages DHIS |
798 |
308 |
665 |
688 |
1 697 |
729 |
|
472 |
287 |
1 047 |
a |
| Hearing aids issued rate |
2022/23 |
both sexes 0-18 years old DHIS |
66,7 |
54,6 |
140,8 |
78,3 |
59,2 |
55,1 |
62,9 |
68,9 |
97,6 |
105,8 |
a |
| both sexes 19 years and older DHIS |
67,0 |
67,6 |
63,9 |
82,6 |
45,8 |
26,4 |
56,3 |
91,9 |
95,6 |
111,7 |
a |
| Prevalence of disability |
2022 |
both sexes 5+ years GHS |
4,8 |
6,6 |
6,6 |
3,9 |
4,1 |
3,7 |
3,9 |
11,5 |
6,3 |
4,9 |
b |
| both sexes all ages Census |
6,0 |
8,5 |
8,4 |
4,9 |
6,1 |
5,0 |
5,1 |
7,6 |
7,0 |
5,4 |
c |
| female 5+ years GHS |
5,3 |
|
|
|
|
|
|
|
|
|
b |
| female all ages Census |
7,0 |
|
|
|
|
|
|
|
|
|
c |
| male 5+ years GHS |
4,2 |
|
|
|
|
|
|
|
|
|
b |
| male all ages Census |
4,9 |
|
|
|
|
|
|
|
|
|
c |
| Prevalence of hearing disability |
2023 |
15 years and older DDI - any functional difficulty |
5,4 |
9,0 |
5,3 |
4,3 |
6,6 |
5,0 |
3,4 |
7,0 |
5,2 |
4,1 |
d |
| Prevalence of sight disability |
2023 |
15 years and older DDI - any functional difficulty |
14,4 |
19,2 |
16,8 |
14,2 |
17,1 |
11,0 |
10,2 |
18,3 |
13,2 |
10,4 |
d |
| Spectacles issued rate |
2022/23 |
both sexes 0-18 years old DHIS |
56,2 |
36,3 |
12,7 |
55,3 |
45,6 |
54,1 |
54,5 |
65,1 |
402,5 |
74,4 |
a |
| both sexes 19 years and older DHIS |
66,2 |
64,4 |
22,5 |
58,0 |
67,6 |
44,7 |
59,2 |
91,8 |
83,4 |
76,5 |
a |
| Wheelchairs issued rate |
2022/23 |
both sexes 0-18 years old DHIS |
65,9 |
41,6 |
103,2 |
68,3 |
61,9 |
48,5 |
69,8 |
24,8 |
85,4 |
97,4 |
a |
| both sexes 19 years and older DHIS |
76,6 |
34,2 |
102,7 |
102,5 |
70,1 |
55,0 |
77,7 |
39,0 |
65,2 |
113,0 |
a |
Reference notes
a webDHIS.16
b Stats SA GHS 2022.34
c Census 2022.33
d The Disability Report 2023.26
Definitions
• Cataract surgery - total [Number]: Number of eyes on which cataract surgery was performed.
• Cataract surgery rate [per 1 million]: Clients who had cataract surgery per 1 million uninsured population.
• Hearing aids issued rate [Percentage]: Hearing aids issued as a proportion of the applications for hearing aids received.
• Prevalence of disability [Percentage]: Percentage of people reporting moderate to severe disability in a survey where disability is defined as a limitation in one or more activities of daily living (seeing, hearing, communication, moving, getting around, daily life activities, learning, intellectual and emotional).
• Prevalence of hearing disability [Percentage]: In the Census questionnaire, respondents were asked to indicate whether or not there were any people with serious visual, hearing, physical or mental disabilities in the household. The seriousness of the disability was not clearly defined. Rather, the respondent’s perceptions of seriousness were relied on.
• Prevalence of sight disability [Percentage]: In the census questionnaire, respondents were asked to indicate whether or not there were any people with serious visual, hearing, physical or mental disabilities in the household. The seriousness of the disability was not clearly defined. Rather, the respondent’s perceptions of seriousness were relied on.
• Spectacles issued rate [Percentage]: Spectacles issued as a % of the applications received.
• Wheelchairs issued rate [Percentage]: Wheelchairs issued as a proportion of the applications for wheelchairs received.
Cataract surgeries
From 2009 to 2016, the Western Cape had the highest rate of cataract operations. However, from 2017 to 2019, the Free State led in cataract surgery rates, rising from 2 140 to 2 628 per 1 million uninsured population. From 2020 to 2022, KwaZulu-Natal had the highest cataract surgery rate, at a time when cataract surgery rates were low across all provinces (Figure 9).

Figure 9.Cataract surgeries per 1 million uninsured population, by province, 2009-2022
The overall number of cataract surgeries performed in all provinces has steadily increased from 49 383 in 2017 to 58 808 in 2019. Although the national number of cataract surgeries increased by approximately 18.7% between 2017 and 2019, this is a consequence of KwaZulu-Natal almost doubling their rate and the Free State increasing the number of surgeries performed in this period. Generally, however, the surgery rate declined across the provinces, with Limpopo experiencing the largest drop in cataract surgery rate (Figure 10). All provinces experienced a reduction in 2020, followed by an increase after 2020. After 2020, KwaZulu-Natal, Gauteng, and the Western Cape showed the greatest recovery in the total number of surgeries performed. Limpopo had the third highest recovery in terms of the rate of cataract surgeries in the same period. Notably, no operations were reported for Mpumalanga after 2019. This pattern matches the issues faced by other South African health facilities during and after the COVID-19 pandemic.

Figure 10.Total number of cataract surgeries performed between 2015 and 2021, by province
Note: No cataract surgeries reported for MP since 2019.
Source: webDHIS.16
Health status indicators
Infectious Disease
Tuberculosis
Global mortality and incidence
The Global Tuberculosis Report 2023 noted that, despite being avoidable and usually curable, TB was the second highest cause of mortality from a single infectious agent in 2022, accounting for nearly twice as many fatalities as HIV.27 In the post-pandemic age, TB is expected to reclaim the top spot. However, the globe is falling short of its TB targets, in part due to disruptions caused by COVID-19. In 2022, TB was expected to kill 1.30 million people worldwide, nearly the same number as in 2019. The WHO End TB Strategy sets a global target of 75% mortality reduction between 2015 and 2025.27 In 2022, the global incidence of TB was expected to be 133 new cases per 100 000 population. In 2022, an estimated 10.6 million people contracted TB. The global treatment gap between the projected number of persons newly infected with TB (incident cases) and the reported number of people diagnosed (notified cases) was 3.1 million.
Local impact and changes in South Africa
The local numbers presented in Table 5 mask a number of significant changes over time. According to WHO, South Africa was one of just 21 countries that had at least a 50% decline in TB incidence between 2015 and 2022, and was the only high-burden country among this group. However, it is sobering to note that South Africa continues to appear on all three high-burden lists for TB, HIV-associated TB, and multi-drug resistant/rifampicin-resistant TB. China, India, Indonesia, Mozambique, Myanmar, Nigeria, the Philippines, and Zambia also appear on all three lists.
Although their impacts will eventually be detectable in the outcome measures reported, the most recently reported figures do not yet show the effects of changes in treatment and prevention regimens that are in the process of being implemented in South Africa. The National Guidelines on the Treatment of Tuberculosis Infection were updated in 2023.65 Notably, these guidelines included expanded access to TB preventive treatment (TPT). In addition, new TPT regimen options were included, including isoniazid and rifapentine given once weekly for three months (3HP) and daily rifampicin and isoniazid for three months (3RH), in addition to the longer isoniazid-only regimens (daily isoniazid for six months (6H) or daily isoniazid for 12 months (12H)). The guideline states that shorter treatment options should be offered where feasible and available.65
Management of rifampicin-resistant TB
The national guidelines for the Clinical Management of Rifampicin-Resistant Tuberculosis (RR-TB) were also updated in 2023.66 South Africa has adopted the WHO recommendation to follow a 6-month, all-oral regimen of bedaquiline, pretomanid and linezolid, with or without moxifloxacin or levofloxacin (BPaLM or BPAL-L). The impact of de-institutionalised and decentralised RR-TB care has yet to be seen in the routine data but will be closely watched. Of note for the indicators reported, the term RR-TB is used in the guidelines to refer to all forms of resistant TB.
Table 5.Tuberculosis indicators
| Indicator |
Period |
Sex|Age|Series|Cat |
SA |
EC |
FS |
GP |
KZ |
LP |
MP |
NC |
NW |
WC |
Ref |
| All DS TB patients in cohort |
2022 |
both sexes DHIS |
205 734 |
45 363 |
9 855 |
30 628 |
47 889 |
13 205 |
11 268 |
7 346 |
11 736 |
28 444 |
a |
| Case detection rate (all forms) |
2022 |
both sexes Global TB (2023) |
77,0 |
|
|
|
|
|
|
|
|
|
b |
| HIV prevalence in TB incident cases |
2022 |
both sexes Global TB |
54,0 |
|
|
|
|
|
|
|
|
|
b |
| Incidence of TB (all types) (per 100 000) |
2022 |
Global TB |
468 |
|
|
|
|
|
|
|
|
|
b |
| Reported cases of MDR TB |
2021 |
WHO |
7 106 |
|
|
|
|
|
|
|
|
|
b |
| 2022 |
WHO |
7 590 |
|
|
|
|
|
|
|
|
|
b |
| Screen for TB symptoms 5 years and older |
2022/23 |
both sexes DHIS |
86 212 706 |
11 136 879 |
3 996 254 |
18 454 955 |
21 848 377 |
10 182 567 |
6 354 327 |
1 904 378 |
4 892 816 |
7 442 153 |
a |
| Screen for TB symptoms under 5 years |
2022/23 |
both sexes DHIS |
17 057 932 |
2 100 216 |
780 122 |
3 286 015 |
4 192 507 |
2 326 579 |
1 536 968 |
343 949 |
962 655 |
1 528 921 |
a |
| TB child under 5 years start on treatment rate |
2022/23 |
DHIS |
97,8 |
98,1 |
87,8 |
97,8 |
99,0 |
105,3 |
98,2 |
91,6 |
105,0 |
96,8 |
a |
| TB client 5 years and older start on treatment rate |
2022/23 |
DHIS |
94,6 |
93,1 |
92,6 |
95,1 |
96,4 |
97,3 |
95,3 |
97,3 |
95,4 |
92,2 |
a |
| TB DS client lost to follow-up rate |
2022 |
both sexes all ages DHIS |
9,8 |
10,1 |
8,4 |
4,6 |
5,9 |
4,8 |
4,7 |
12,3 |
4,1 |
28,1 |
a |
| TB DS death rate |
2022 |
both sexes all ages DHIS |
5,6 |
5,1 |
9,4 |
5,5 |
4,9 |
9,1 |
6,1 |
5,6 |
5,6 |
4,2 |
a |
| TB DS treatment success rate |
2021 |
both sexes all ages DHIS |
77,9 |
76,6 |
71,3 |
82,5 |
82,1 |
78,9 |
82,8 |
64,9 |
82,1 |
73,0 |
a |
| Global TB |
79,0 |
|
|
|
|
|
|
|
|
|
b |
| 2022 |
both sexes all ages DHIS |
59,3 |
54,5 |
52,5 |
56,4 |
55,7 |
50,4 |
56,3 |
55,1 |
61,7 |
84,1 |
a |
| TB MDR client death rate |
2021 |
DHIS |
16,6 |
18,1 |
24,4 |
14,8 |
14,8 |
18,9 |
16,2 |
20,6 |
21,2 |
14,4 |
a |
| TB MDR treatment success rate |
2020 |
both sexes all ages Global TB |
62,0 |
|
|
|
|
|
|
|
|
|
b |
| 2021 |
both sexes all ages DHIS |
54,1 |
53,1 |
53,0 |
60,7 |
57,2 |
57,9 |
63,3 |
49,8 |
64,5 |
43,4 |
a |
| TB symptom 5 years and older screened in facility rate |
2022/23 |
both sexes DHIS |
97,6 |
93,5 |
93,3 |
112,7 |
105,9 |
97,8 |
96,2 |
88,0 |
84,0 |
73,4 |
a |
| TB symptom child under 5 years screened in facility rate |
2022/23 |
both sexes DHIS |
94,5 |
95,4 |
100,8 |
98,0 |
102,6 |
88,4 |
100,4 |
92,0 |
81,9 |
79,5 |
a |
| TB mortality rate per 100 000 |
2021 |
both sexes all ages Global TB |
93,0 |
|
|
|
|
|
|
|
|
|
b |
| 2022 |
both sexes all ages Global TB |
90,0 |
|
|
|
|
|
|
|
|
|
b |
| TB mortality rate per 100 000 (excluding HIV) |
2021 |
Global TB |
38,0 |
|
|
|
|
|
|
|
|
|
b |
| 2022 |
Global TB |
39,0 |
|
|
|
|
|
|
|
|
|
b |
Reference notes
a webDHIS.16
b Global TB database.67
Definitions
• All DS TB patients in cohort. [Number]
• Screen for TB symptoms 5 years and older [Number]: Clients 5 years and older who were screened in health facilities for TB symptoms using the standard TB screening tool as per National TB Guidelines.
• Screen for TB symptoms under 5 years [Number]: Children under 5 years who were screened in health facilities for TB symptoms using the standard TB screening tool as per National TB Guideline.
• TB child under 5 years start on treatment rate [Percentage]: TB client under 5 years started on treatment as a proportion of ALL symptomatic children under 5 years.
• TB client 5 years and older start on treatment rate [Percentage]: TB client 5 years and older start on treatment as a proportion of TB symptomatic client 5 years and older test positive.
• TB DS client lost to follow-up rate [Percentage]: The percentage of TB clients (all types of TB) who defaulted on treatment.
• TB DS death rate [Percentage]: The percentage of TB clients (all types of TB registered in ETR.net) who died.
• TB DS treatment success rate [Percentage]: The percentage of TB clients (all types registered in ETR.net) cured plus those who completed treatment.
• TB MDR client death rate [Percentage]: The percentage of TB clients (MDR TB) who died.
• TB MDR client loss to follow-up rate [Percentage]: The percentage of TB clients (MDR TB) who are lost to follow up.
• TB MDR treatment success rate [Percentage]: The percentage of TB clients (MDR TB) cured plus those who completed treatment.
• TB symptom child under 5 years screened in facility rate [Percentage]: Children under 5 years screened for TB symptoms as a proportion of PHC headcount under 5 years.
• Tuberculosis mortality rate per 100 000 (excluding HIV) [per 100 000 population]: Number of deaths due to tuberculosis (all types) reported per 100 000 population (for the year). The reported TB mortality excludes deaths occurring in HIV-positive TB cases, in accordance with the definition used in ICD-10.
• Tuberculosis mortality rate per 100 000 [per 100 000 population]: Number of deaths due to tuberculosis (all types) reported per 100 000 population (for the year).
HIV
Progress towards global targets
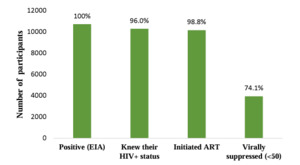
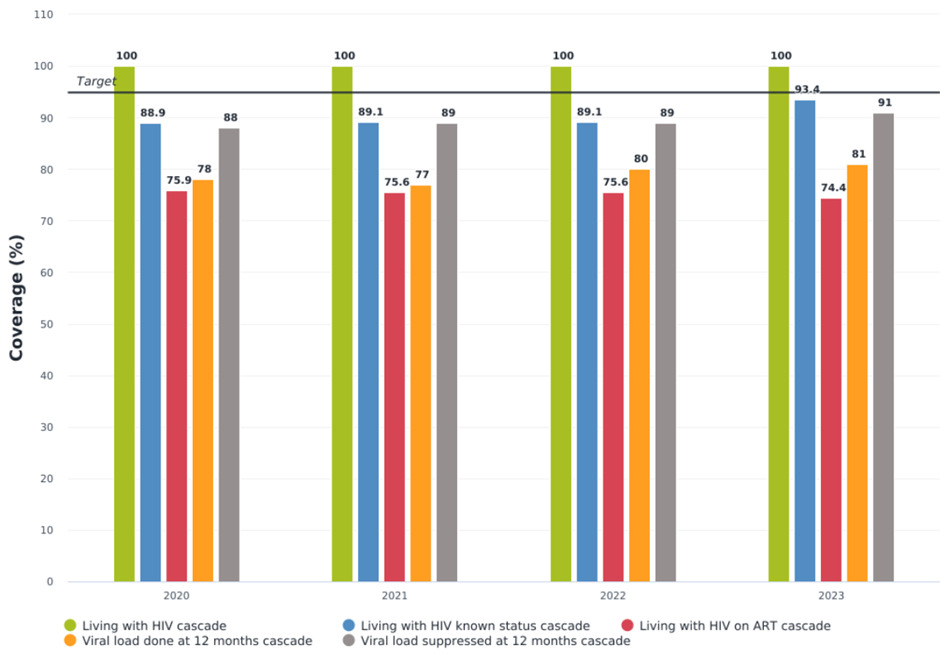
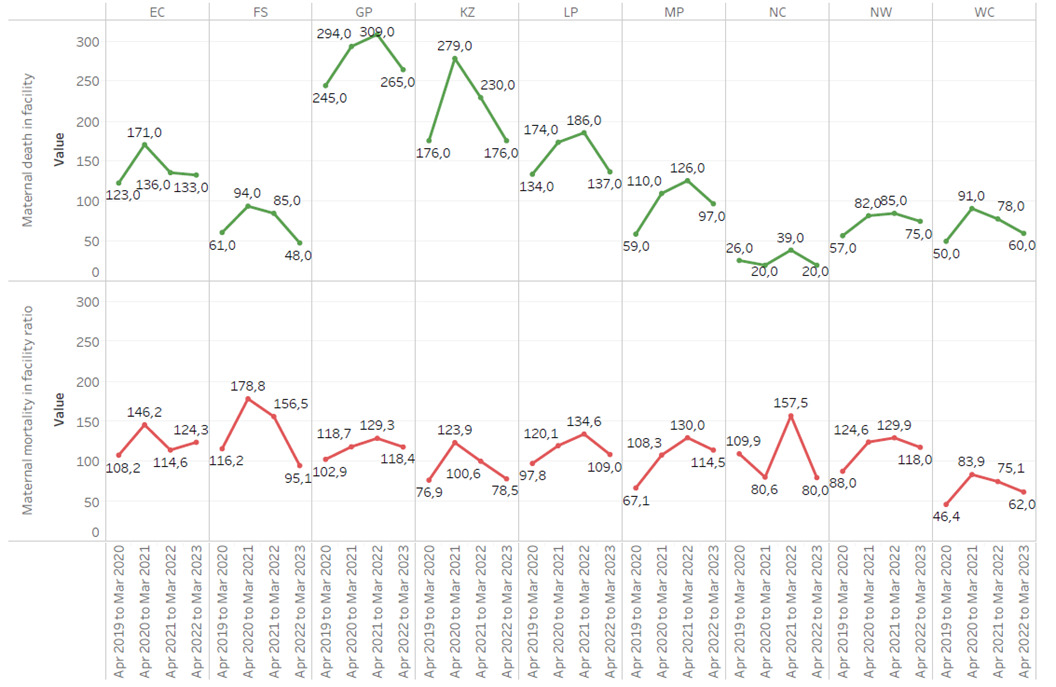
South Africa adopted WHO’s Universal Test and Treat (UTT) recommendation in 2016.68 The UTT standards support the UNAIDS 90-90-90 treatment target to end the AIDS pandemic, which has now been revised to 95-95-95. The initial target was that by 2020, 90% of PLHIV would know their status, 90% of those would be on antiretroviral treatment (ART), and 90% of those on treatment would achieve viral suppression. WebDHIS reported figures of 89-76-88 for South Africa in 2020.16 Despite the UTT recommendations, South Africa failed to meet ART uptake and virus suppression targets, with only 78% virally suppressed.29 Figure 11 shows progress towards the 2030 goal of 95-95-95.
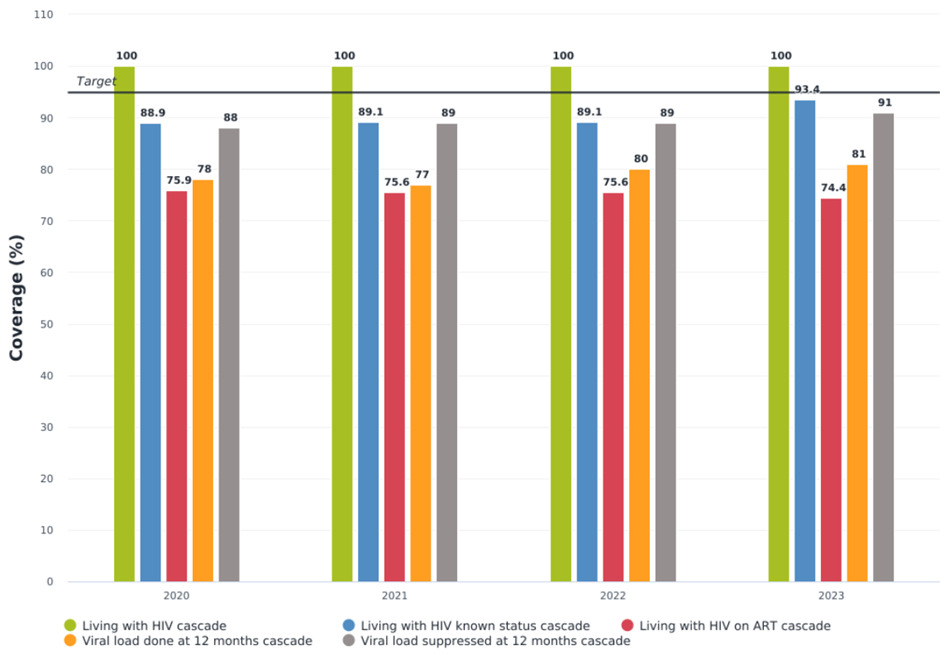
Figure 11.National HIV 95:95:95 test and treat estimates, 2020-2023
UTT estimates as of the 2022/23 financial year reported by the Thembisa model v4.6,69 the Sixth South African National HIV Prevalence, Incidence, Behaviour and Communication Survey (SABSSM VI),35 and the Antenatal Survey of Pregnant Women36 across both sexes and at varying age ranges are presented in Figure 12.

Figure 12.HIV test and treat estimates by province, 2022-2023
Sources: Thembisa v4.6,69 SABSSM VI,35 Antenatal Survey of Pregnant Women.36
The steady decline in almost all epidemic estimates demonstrates the benefits of HIV services provided in accordance with UTT recommendations. The number of new HIV infections fell from 210 000 in 2021 to 160 000 in 2022, across all ages. AIDS-related deaths declined from 51 000 in 2021 to 45 000 in 2022. However, as treatment access improves, prevalence also increases. In 2021 and 2022, the number of PLHIV increased from 7.5 million to 7.6 million. Table 6 presents additional provincial HIV indicators.29,70
Women aged 15 to 49 continue to have higher infection rates than other age groups. In 2021 and 2022, this group reported 130 000 and 100 000 new cases, respectively.29,70 According to a recent Human Sciences Research Council national population survey, age-disparate relationships, limited access to testing and treatment facilities, and a lack of condom use may increase the burden on the 15-49-year-old demographic.71–73 Continued focus on disaggregated data relevant to this and other vulnerable groups is therefore critical.
Table 6.HIV indicators by province
| Indicator |
Period |
Sex|Age|Series|Cat |
SA |
EC |
FS |
GP |
KZ |
LP |
MP |
NC |
NW |
WC |
Ref |
| Child living with HIV |
2023 Q1 |
both sexes 0-14 years NDoH-Thembisa |
233 948 |
27 277 |
13 990 |
43 362 |
63 774 |
25 242 |
25 800 |
3 815 |
16 676 |
14 012 |
a |
| Adult living with HIV |
2023 Q1 |
both sexes 15+ years NDoH-Thembisa |
7 741 997 |
881 465 |
404 915 |
1 823 564 |
1 990 038 |
687 920 |
733 926 |
109 798 |
532 481 |
577 890 |
a |
| Total living with HIV |
2023 Q1 |
both sexes all ages NDoH-Thembisa |
7 975 945 |
908 742 |
418 905 |
1 866 926 |
2 053 812 |
713 162 |
759 726 |
113 613 |
549 157 |
591 902 |
a |
| People living with HIV (PLHIV) |
2022 |
both sexes 0-14 years Global report |
230 000 |
|
|
|
|
|
|
|
|
|
b |
| both sexes 15 years and older SABSSM VI |
7 400 000 |
|
|
|
|
|
|
|
|
|
c |
| both sexes all ages Global report |
7 600 000 |
|
|
|
|
|
|
|
|
|
b |
| both sexes all ages SABSSM VI |
7 800 000 |
|
|
|
|
|
|
|
|
|
c |
| female 15 years and older Global report |
4 800 000 |
|
|
|
|
|
|
|
|
|
b |
| male 15 years and older Global report |
2 600 000 |
|
|
|
|
|
|
|
|
|
b |
| 2023 |
both sexes all ages Thembisa 4.6 |
7 850 920 |
880 306 |
428 498 |
1 906 310 |
1 975 690 |
715 780 |
753 263 |
105 791 |
541 410 |
530 089 |
d |
| HIV prevalence (age 15-49) |
2022 |
both sexes 15-49 years Global report |
17,8 |
|
|
|
|
|
|
|
|
|
b |
| both sexes 15-49 years SABSSM VI |
17,0 |
|
|
|
|
|
|
|
|
|
c |
| both sexes mid-year |
19,6 |
|
|
|
|
|
|
|
|
|
e |
| female 15-49 years SABSSM VI |
22,3 |
|
|
|
|
|
|
|
|
|
c |
| male 15-49 years SABSSM VI |
11,0 |
|
|
|
|
|
|
|
|
|
c |
| HIV prevalence (total population) |
2022 |
both sexes 15 years and older SABSSM VI |
16,3 |
18,8 |
19,1 |
15,0 |
21,8 |
11,9 |
20,8 |
10,0 |
16,5 |
8,2 |
c |
| both sexes all ages SABSSM VI |
12,7 |
|
|
|
|
|
|
|
|
|
c |
| both sexes all ages Thembisa 4.6 |
13,2 |
13,5 |
15,0 |
11,9 |
17,6 |
11,8 |
15,8 |
9,4 |
13,2 |
7,4 |
d |
| both sexes mid-year |
13,9 |
|
|
|
|
|
|
|
|
|
e |
| Global report Men who sex with men |
29,7 |
|
|
|
|
|
|
|
|
|
b |
| Global report People who inject drugs |
21,8 |
|
|
|
|
|
|
|
|
|
b |
| Global report Prisoners |
7,0 |
|
|
|
|
|
|
|
|
|
b |
| Global report Sex workers |
62,3 |
|
|
|
|
|
|
|
|
|
b |
| Global report Transgender people |
58,0 |
|
|
|
|
|
|
|
|
|
b |
| Percentage of PLHIV who know their status (1st 90) |
2022 |
both sexes 0-14 years Global report |
83,0 |
|
|
|
|
|
|
|
|
|
b |
| both sexes 15 years and older SABSSM VI |
90,0 |
|
|
|
|
|
|
|
|
|
c |
| female 15 years and older Global report |
95,0 |
|
|
|
|
|
|
|
|
|
b |
| female 15 years and older SABSSM VI |
92,0 |
|
|
|
|
|
|
|
|
|
c |
| female 15-49 years Antenatal Survey Pregnant women |
96,0 |
78,4 |
79,2 |
74,6 |
99,3 |
73,7 |
78,5 |
76,6 |
79,7 |
80,0 |
f |
| male 15 years and older Global report |
94,0 |
|
|
|
|
|
|
|
|
|
b |
| male 15 years and older SABSSM VI |
85,0 |
|
|
|
|
|
|
|
|
|
c |
| Child ART Total |
Mar 2023 |
both sexes 0-14 years DHIS |
111 783 |
14 608 |
6 724 |
17 866 |
31 389 |
11 031 |
11 940 |
3 696 |
7 434 |
7 095 |
a |
| Adult ART Total |
Mar 2023 |
both sexes 15+ years DHIS |
5 326 130 |
579 407 |
306 549 |
1 208 516 |
1 529 901 |
419 601 |
551 195 |
65 167 |
351 048 |
314 746 |
a |
| Number of patients receiving ART |
2023 |
both sexes all ages Thembisa 4.6 |
5 871 150 |
621 890 |
327 004 |
1 359 860 |
1 634 970 |
454 937 |
583 548 |
73 450 |
384 186 |
357 298 |
d |
| Total Clients remaining on ART at the end of the month |
Mar 2023 |
both sexes all ages DHIS |
5 437 913 |
594 015 |
313 273 |
1 226 382 |
1 561 290 |
430 632 |
563 135 |
68 863 |
358 482 |
321 841 |
a |
| Clients remaining on ART rate |
Mar 2023 |
both sexes all ages DHIS |
68,2 |
65,4 |
74,8 |
65,7 |
76,0 |
60,4 |
74,1 |
60,6 |
65,3 |
54,4 |
a |
| Antiretroviral coverage (2nd 90) |
2022 |
both sexes 0-14 years Global report |
54,0 |
|
|
|
|
|
|
|
|
|
b |
| both sexes 15 years and older SABSSM VI |
91,0 |
|
|
|
|
|
|
|
|
|
c |
| both sexes all ages med schemes |
77,5 |
|
|
|
|
|
|
|
|
|
g |
| both sexes all ages Thembisa 4.6 |
73,2 |
69,3 |
75,1 |
69,6 |
81,4 |
62,3 |
75,9 |
68,2 |
69,4 |
65,9 |
d |
| female 15 years and older Global report |
80,0 |
|
|
|
|
|
|
|
|
|
b |
| female 15 years and older SABSSM VI |
91,0 |
|
|
|
|
|
|
|
|
|
c |
| female 15-49 years Antenatal Survey Pregnant women |
98,8 |
83,0 |
88,9 |
83,5 |
84,8 |
84,1 |
88,9 |
86,6 |
88,9 |
72,8 |
f |
| female all ages Thembisa 4.6 |
78,0 |
|
|
|
|
|
|
|
|
|
d |
| female Global report Pregnant women |
98,0 |
|
|
|
|
|
|
|
|
|
b |
| Global report Men who sex with men |
44,1 |
|
|
|
|
|
|
|
|
|
b |
| Global report Prisoners |
99,3 |
|
|
|
|
|
|
|
|
|
b |
| Global report Sex workers |
69,5 |
|
|
|
|
|
|
|
|
|
b |
| male 15 years and older Global report |
68,0 |
|
|
|
|
|
|
|
|
|
b |
| male 15 years and older SABSSM VI |
90,0 |
|
|
|
|
|
|
|
|
|
c |
| males all ages Thembisa 4.6 |
65,4 |
|
|
|
|
|
|
|
|
|
d |
| 2023 |
both sexes all ages Thembisa 4.6 |
74,8 |
70,7 |
76,3 |
71,4 |
82,8 |
63,6 |
77,5 |
69,4 |
71,0 |
67,4 |
d |
| Child with viral load suppressed rate 12 months |
2023 Q1 |
both sexes 0-14 years DHIS |
60,1 |
64,9 |
58,5 |
52,9 |
66,3 |
54,8 |
58,7 |
50,0 |
61,4 |
71,0 |
a |
| Adult with viral load suppressed rate 12 months |
2023 Q1 |
both sexes 15+ years DHIS |
90,6 |
90,6 |
91,2 |
89,4 |
91,4 |
89,8 |
91,7 |
86,4 |
89,6 |
93,4 |
a |
| ART client viral load suppressed rate (VLS) |
2023 Q1 |
both sexes all ages DHIS-Tier |
90,0 |
90,0 |
90,0 |
89,0 |
91,0 |
89,0 |
91,0 |
85,0 |
89,0 |
93,0 |
a |
| HIV viral load suppression (3rd 90) |
2022 |
both sexes 0-14 years Global report |
37,0 |
|
|
|
|
|
|
|
|
|
b |
| both sexes 0-14 years Thembisa 4.6 |
35,1 |
36,3 |
37,6 |
29,0 |
40,1 |
27,2 |
35,1 |
40,4 |
32,5 |
48,9 |
d |
| both sexes 15 years and older SABSSM VI |
81,2 |
80,2 |
81,2 |
79,1 |
86,7 |
75,3 |
82,2 |
78,2 |
76,8 |
78,8 |
c |
| both sexes 15-24 years SABSSM VI |
70,1 |
|
|
|
|
|
|
|
|
|
c |
| both sexes 15-49 years SABSSM VI |
79,5 |
|
|
|
|
|
|
|
|
|
c |
| both sexes 25-49 years SABSSM VI |
80,5 |
|
|
|
|
|
|
|
|
|
c |
| both sexes all ages Thembisa 4.6 |
65,4 |
61,0 |
69,7 |
62,6 |
75,2 |
55,1 |
68,5 |
61,9 |
62,5 |
61,4 |
d |
| female 15 years and older Global report |
74,0 |
|
|
|
|
|
|
|
|
|
b |
| female 15 years and older SABSSM VI |
82,9 |
|
|
|
|
|
|
|
|
|
c |
| female 15-19 years Antenatal Survey Pregnant women |
46,0 |
|
|
|
|
|
|
|
|
|
f |
| female 15-24 years SABSSM VI |
68,2 |
|
|
|
|
|
|
|
|
|
c |
| female 15-49 years Antenatal Survey Pregnant women |
74,1 |
70,7 |
76,7 |
72,6 |
81,3 |
59,9 |
71,9 |
53,7 |
66,0 |
76,3 |
f |
| female 15-49 years SABSSM VI |
81,6 |
|
|
|
|
|
|
|
|
|
c |
| female 25-49 years SABSSM VI |
82,8 |
|
|
|
|
|
|
|
|
|
c |
| female 30-34 years Antenatal Survey Pregnant women |
77,1 |
|
|
|
|
|
|
|
|
|
f |
| male 15 years and older Global report |
62,0 |
|
|
|
|
|
|
|
|
|
b |
| male 15 years and older SABSSM VI |
77,6 |
|
|
|
|
|
|
|
|
|
c |
| male 15 years and older Thembisa 4.6 |
58,6 |
|
|
|
|
|
|
|
|
57,2 |
d |
| male 15-24 years SABSSM VI |
73,5 |
|
|
|
|
|
|
|
|
|
c |
| male 15-49 years SABSSM VI |
74,8 |
|
|
|
|
|
|
|
|
|
c |
| male 25-49 years SABSSM VI |
74,9 |
|
|
|
|
|
|
|
|
|
c |
| Antiretroviral effective coverage |
2023 Q1 |
both sexes 0-14 years DHIS-Tier |
21,2 |
20,2 |
19,2 |
17,4 |
26,8 |
19,1 |
22,3 |
17,6 |
23,9 |
11,6 |
a |
| both sexes 15+ years DHIS-Tier |
47,2 |
40,8 |
49,2 |
46,4 |
58,2 |
45,2 |
57,5 |
18,5 |
50,5 |
11,5 |
a |
| both sexes all ages DHIS-Tier |
46,4 |
40,2 |
48,2 |
45,8 |
57,2 |
44,3 |
56,3 |
18,4 |
49,7 |
11,5 |
a |
| Infant PCR test positive around 10 weeks rate |
2022/23 |
both sexes DHIS |
0,4 |
0,6 |
0,4 |
0,5 |
0,3 |
0,5 |
0,5 |
0,8 |
0,3 |
0,2 |
a |
| Adult living with HIV viral load done 12m |
2020 Q1 |
both sexes 15+ years DHIS-Tier |
3 403 846 |
352 021 |
179 121 |
886 716 |
1 055 123 |
286 134 |
406 715 |
16 964 |
221 052 |
|
a |
| 2021 Q1 |
15+ years DHIS |
3 734 509 |
377 554 |
198 456 |
898 715 |
1 111 108 |
292 891 |
396 112 |
27 698 |
255 405 |
176 570 |
a |
| 2022 Q1 |
15+ years DHIS |
3 899 389 |
391 707 |
214 659 |
924 923 |
1 210 061 |
312 055 |
425 359 |
27 427 |
273 492 |
119 706 |
a |
| Adult living with HIV viral load suppressed (VLS) 12m |
2021 Q1 |
both sexes 15+ years DHIS |
3 317 696 |
334 432 |
178 051 |
799 532 |
992 743 |
258 942 |
350 454 |
23 238 |
220 859 |
159 445 |
a |
| 2022 Q1 |
both sexes 15+ years DHIS |
3 464 855 |
339 499 |
199 254 |
844 446 |
1 095 505 |
249 401 |
373 072 |
23 306 |
230 668 |
109 704 |
a |
| 2023 Q1 |
both sexes 15+ years DHIS |
3 651 215 |
359 480 |
199 143 |
846 568 |
1 157 385 |
310 917 |
421 941 |
20 265 |
268 959 |
66 557 |
a |
| Adult remaining on ART at end of the month - total |
Mar 2023 |
both sexes 15+ years DHIS |
5 326 130 |
579 407 |
306 549 |
1 208 516 |
1 529 901 |
419 601 |
551 195 |
65 167 |
351 048 |
314 746 |
a |
| Antenatal client initiated on ART rate |
2022/23 |
female DHIS |
94,1 |
89,8 |
95,1 |
99,8 |
96,6 |
97,3 |
99,1 |
90,0 |
94,6 |
63,3 |
a |
| Child under 15 years remaining on ART at end of the month - total |
Mar 2023 |
both sexes 15+ years DHIS |
111 783 |
14 608 |
6 724 |
17 866 |
31 389 |
11 031 |
11 940 |
3 696 |
7 434 |
7 095 |
a |
| HIV prevalence among antenatal clients |
2022 |
15-19 years Antenatal Survey |
7,6 |
|
|
|
|
|
|
|
|
|
f |
| 15-24 years Antenatal Survey |
13,6 |
|
|
|
|
|
|
|
|
|
f |
| 15-49 years Antenatal Survey |
27,5 |
32,9 |
30,3 |
26,4 |
37,2 |
19,4 |
30,8 |
15,2 |
25,7 |
16,3 |
f |
| 20-24 years Antenatal Survey |
16,4 |
|
|
|
|
|
|
|
|
|
f |
| Infant 1st PCR test positive at birth rate |
2022/23 |
both sexes DHIS |
0,4 |
0,5 |
0,3 |
0,5 |
0,4 |
0,5 |
0,2 |
0,4 |
0,5 |
0,9 |
a |
| Male circumcision (% of men who are circumcised) |
2022 |
15-49 years THEMBISA 4.6 |
62,5 |
78,7 |
64,4 |
71,4 |
56,1 |
91,3 |
77,4 |
38,5 |
53,2 |
44,4 |
d |
| male 15-24 years SABSSM VI |
49,9 |
|
|
|
|
|
|
|
|
|
c |
| male 25-34 years SABSSM VI |
44,4 |
|
|
|
|
|
|
|
|
|
c |
| male 35-44 years SABSSM VI |
37,9 |
|
|
|
|
|
|
|
|
|
c |
| male 45-54 years SABSSM VI |
25,7 |
|
|
|
|
|
|
|
|
|
c |
| male 55-64 years SABSSM VI |
25,2 |
|
|
|
|
|
|
|
|
|
c |
| male 65+ years SABSSM VI |
21,8 |
|
|
|
|
|
|
|
|
|
c |
| Medical male circumcision 10 years and older |
2022/23 |
male 10+ years DHIS |
369 483 |
5 835 |
17 955 |
79 727 |
144 750 |
22 130 |
57 315 |
7 478 |
20 967 |
13 326 |
a |
| Medical male circumcision 10-14 years rate |
2022/23 |
male 10-14 years DHIS |
49,4 |
23,6 |
48,5 |
56,4 |
59,9 |
51,9 |
35,5 |
59,0 |
16,5 |
7,4 |
a |
| Medical male circumcision 15 years and older rate |
2022/23 |
DHIS |
50,6 |
76,4 |
51,5 |
43,6 |
40,1 |
48,1 |
64,5 |
41,0 |
83,5 |
92,6 |
a |
Reference notes
a webDHIS.16
b UNAIDS 2023.29
c HIV Household Survey 2022.35
d Thembisa 4.6.69
e Stats SA MYE 2022.74
f Antenatal Survey 2022.73
g Medical schemes 2022.48
Definitions
• Adult ART Total [Number].
• Adult living with HIV [Number]: Estimated number of adults (15+ years) living with HIV.
• Adult remaining on ART at end of the month - total [Number].
• Child ART Total [Number].
• Child living with HIV [Number]: Estimated number of children (0-14 years) living with HIV.
• Child under 15 years remaining on ART at end of the month - total [Number].
• Medical male circumcision 10 years and older [Number]: Males 10 years and older who are circumcised under medical supervision.
• Number of patients receiving ART [Number]: Number of patients receiving ART.
• People living with HIV (PLHIV) [Number]: The number of people who are HIV-positive.
• Total clients remaining on ART at the end of the month [Number].
• Total living with HIV [Number]: The estimated number of people who are HIV-positive.
• Antenatal client initiated on ART rate [Percentage]: Antenatal clients on ART as a proportion of the total number of antenatal clients who are HIV positive and not previously on ART.
• Antiretroviral coverage (2nd 90) [Percentage]: The number of patients receiving ART, divided by the number needing treatment. The denominator has changed over time, due to changes in treatment guidelines affecting the criteria for treatment eligibility. The latest definition is that all HIV-infected patients should be on ART. This indicator is also one of the 95-9-95 global targets for AIDS (UNAIDS).
• Antiretroviral effective coverage [Percentage]: Proportion of HIV-positive people on ART and virally suppressed. Any implausible values (>100) capped at 100, zero or missing values set to 1.
• ART client viral load suppressed rate (VLS) [Percentage]: ART viral load suppressed - total as a proportion of ART viral load done - total.
• Child with viral load suppressed rate 12 months [Percentage]: Proportion of ART clients with viral load suppressed at different time intervals. This indicates the population level immunological impact of clients on ART.
• Clients remaining on ART rate [Percentage]: Percentage of estimated people living with HIV who remain on ART. (Routine data equivalent for Antiretroviral coverage).
• HIV prevalence (age 15-49) [Percentage]: Percentage of population (age 15-49) estimated to be HIV-positive.
• HIV prevalence (total population) [Percentage]: Percentage of population estimated to be HIV positive. WHO Core indicator is given per 1000 population rather than %.
• HIV prevalence among antenatal clients [Percentage]: Percentage of women surveyed testing positive for HIV.
• HIV viral load suppression (3rd 90) [Percentage]: Percentage of people on ART who are virologically suppressed (VL level <= 1000 copies/mL). This indicator is also one of the 95-95-95 global targets for AIDS (UNAIDS).
• Infant 1st PCR test positive at birth rate [Percentage]: Infants tested PCR positive for the first time at birth as proportion of infants PCR tested at birth.
• Infant PCR test positive around 10 weeks rate [Percentage]: Infants tested PCR positive for follow up test as a proportion of Infants PCR tested around 10 weeks.
• Male circumcision (% of men who are circumcised) [Percentage]: The percentage of men (15-59 years, unless otherwise specified) who have been circumcised.
• Medical male circumcision 10-14 years rate [Percentage]: Medical male circumcisions performed 10-14 years as a proportion of total medical male circumcisions performed.
• Medical male circumcision 15 years and older rate [Percentage]: Medical male circumcisions performed 15 years and older as a proportion of total medical male circumcisions performed.
• Percentage of people living with HIV (PLHIV) who know their status (1st 90) [Percentage]: Percentage of people living with HIV who know their HIV status. This indicator is also one of the 95-95-95 global targets for AIDS (UNAIDS).
Retention on ART
At the end of March 2023, a total of 5 326 130 adults and adolescents in South Africa were reported to be on ART in the public sector, according to webDHIS.16 KwaZulu-Natal had the most patients on ART, with 1 529 901, while the Northern Cape had the fewest, with 65 167 (Figure 13). In addition, 111 783 paediatric patients were reported to be on ART. Figure 14 shows that 31 389 paediatric patients were from KwaZulu-Natal, while only 3 696 were from the Northern Cape.

Figure 13.Total number of adults remaining on ART by province, 2022/23
The 2017 and 2019 National Prenatal HIV Sentinel Surveys reported results of 96-87-64 and 98-96-66, respectively, for the 90-90-90 HIV objectives among prenatal patients by the end of 2020. The 2022 survey findings, which included 10 726 participants, revealed that 96% (10 300) of these women already knew they were living with HIV before being screened at an antenatal visit. Of those who knew their status, 99% (10 166) had already started on ART, and 74% were virally suppressed.75 Thus, while the second 95 target had already been met by 2022 in pregnant women, the third 95 target, related to viral suppression, showed a concerning deficit, as depicted in Figure 15.

Figure 14.HIV care cascade among antenatal women, 2022
Source: HIV Antenatal Survey, 2022.36
The shift to a Dolutegravir (DTG) containing first-line ART regimen in December 2019 was done due to an expected improvement in adherence and also viral suppression.76 A study conducted by Asare et al.,77 in 2024 in the eThekwini municipality, involving patients transitioned between December 2019 and November 2020, demonstrated that DTG-based regimens were associated with comparable or superior retention in care and enhanced viral suppression when compared to the previously recommended treatment protocols. Figure 16 shows KwaZulu-Natal had the highest uptake (80.8%) of the DTG-based regimen in antenatal women, with uptake the lowest in the Northern Cape (35.6%). It will be critical to monitor prenatal viral loads at both national and provincial levels, in order to track progress against the targets.36

Figure 15.ART treatment coverage by regimen type among antenatal women, 2022
Source: HIV Antenatal Survey.36
HIV drug resistance
Antiretroviral drugs are at risk of being partially or fully inactive against HIV, due to the ever evolving genetic structure of HIV.78 Inability to reach viral suppression targets due to HIV drug resistance (HIVDR) can have human cost and negative impacts on the national health budget. WHO’s Africa Regional Action Plan 2019-2023 was intended to monitor and actively conduct HIVDR surveillance in Africa through nationally representative surveys.79 From 2014 to 2016, the only South African data reported were for infants under 18 months of age, with 63.7% resistance to efavirenz or nevirapine. Other populations have been surveyed outside of South Africa.
While South Africa and other low- and middle-income countries have employed DTG to combat HIVDR, more regular nationally representative surveys are required for effective HIVDR surveillance. The HIV indicators by province are captured in Table 6.
Maternal and reproductive health
Table 7 presents the maternal and reproductive health indicators by province for the financial year 2022/23.
Maternal mortality
The number of maternal deaths that occurred in public health institutions peaked in 2020/21, and then began to decrease in 2021/22. As depicted to Figure 20, the number of maternal deaths was highest in Gauteng, while the Northern Cape recorded the lowest number. Since the COVID-19 pandemic, maternal mortality rates have decreased, perhaps indicating that maternal services have recovered. Likewise, the maternal mortality ratio (MMR) per 100 000 live births peaked in 2020/21 and then declined in 2021/2022. The MMR was highest in the Free State in 2020/21 (178.8 per 100 000 live births). In 2021/22, the MMR was highest in the North West province (129.9 per 100 000 live births). Following the COVID-19 pandemic, the MMR and the number of maternal deaths continue to decrease, as shown in Figure 20.
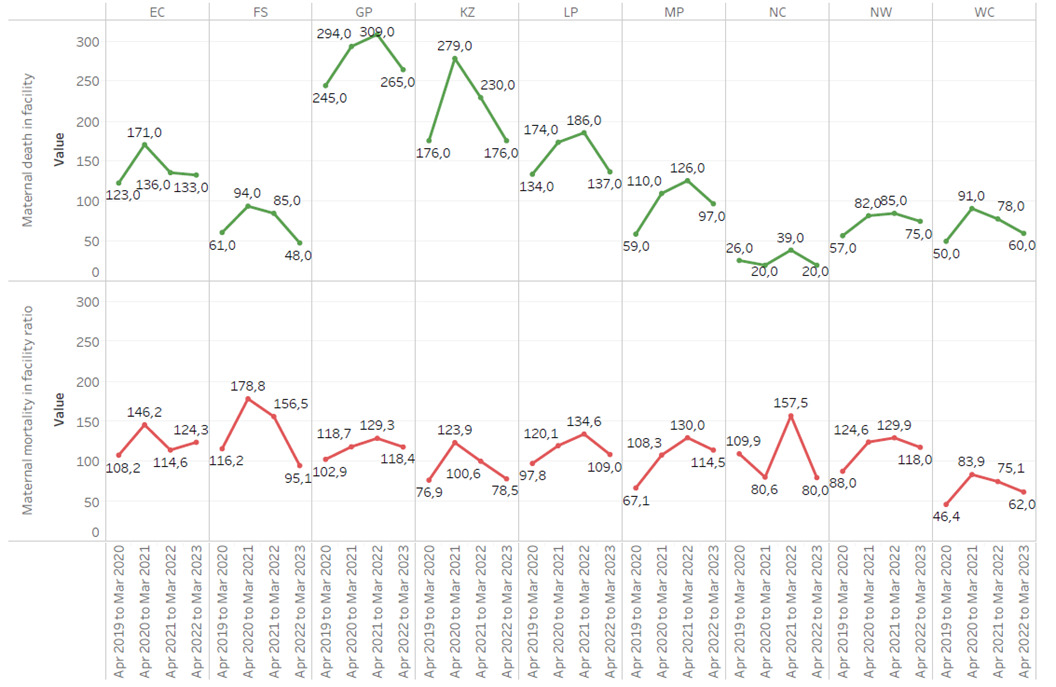
Figure 16.In-facility maternal deaths and maternal mortality facility ratio
Condoms
A recent Spotlight NSP report, based on data from the District Health Barometer, revealed a substantial drop in condom distribution in South Africa over the past five years.80 Contrary to this tendency, female condom distribution was steadily increasing prior to the epidemic. Figure 17 depicts how the distribution of female condoms grew dramatically across most areas following the pandemic. Data from the Thembisa 4.2 and 4.6 models demonstrate a consistent increase in condom use during last sexual encounter among both sexes in the 15-24 and 15-49 age groups, despite disruptions in health care due to COVID-19.69

Figure 17.Female condoms distributed by province, 2019-2023
Teenage pregnancy
According to Stats SA General Household Survey reports, teenage pregnancy steadily ranged between 5.1-5.7% from 2017 to 201934, reaching a high of 5.7% at the beginning of the COVID-19 pandemic as shown in Figure 18. Although there was a declining trend from 2019 to 2021, there was a sharp increase in 2022. Teenage pregnancy is associated with poor access to contraceptive services, risky behaviour, coercive and unprotected sexual contact, and increased exposure to sexually transmissible infections.81 Unwanted pregnancies in teenage mothers are therefore indicative of poor access to sexual and reproductive health rights and services.

Figure 18.Percentage of pregnant 14-19-year-old females, 2017-2023
Data for 2020 not reported
Source: GHS.34
From 2020 to 2023, South Africa experienced slight declines in the number of births occurring in healthcare facilities under supervision of trained staff, as shown in Figure 19. This trend warrants monitoring, given reports of mistreatment of pregnant women.82,83 Anxieties about attending health facilities during the COVID-19 pandemic most likely contributed to reduced in-facility live births between 2020 and 2022. Marginal recovery post-COVID-19 in some provinces suggests that fear of contracting COVID-19, and other structural factors such as lack of transport, potentially persist.84

Figure 19.Live births in facility by province, 2019 - 2023
The maternal and reproductive health indicators are presented in Table 7.
Table 7.Maternal and reproductive health indicators by province
| Indicator |
Period |
Sex|Age|Series|Cat |
SA |
EC |
FS |
GP |
KZ |
LP |
MP |
NC |
NW |
WC |
Ref |
| Antenatal 1st visit before 20 weeks rate |
2022 |
female 15-49 years Antenatal Survey |
61,0 |
55,0 |
59,9 |
56,6 |
64,5 |
60,7 |
57,1 |
59,8 |
65,2 |
71,9 |
a |
| 2022/23 |
female DHIS |
70,1 |
63,5 |
62,1 |
69,3 |
73,8 |
67,5 |
77,3 |
58,5 |
71,2 |
74,3 |
b |
| Antenatal 1st visit coverage |
2022/23 |
female DHIS |
76,4 |
74,8 |
75,4 |
76,1 |
75,1 |
80,1 |
78,1 |
91,2 |
69,6 |
78,6 |
b |
| Cervical cancer screening coverage |
2022/23 |
female DHIS |
21,4 |
22,7 |
24,0 |
16,9 |
38,9 |
12,0 |
24,7 |
9,6 |
9,7 |
17,4 |
b |
| Condom use at last sex |
2022 |
15-24 years THEMBISA 4.6 |
35,4 |
28,3 |
33,2 |
40,8 |
33,7 |
25,9 |
32,5 |
25,5 |
37,4 |
30,8 |
c |
| 25-49 years THEMBISA 4.6 |
26,1 |
23,1 |
25,5 |
27,7 |
28,1 |
20,8 |
26,4 |
20,6 |
27,7 |
20,9 |
c |
| female 15-24 years SABSSM VI |
43,5 |
|
|
|
|
|
|
|
|
|
d |
| female 25-49 years SABSSM VI |
40,9 |
|
|
|
|
|
|
|
|
|
d |
| female 50+ years SABSSM VI |
29,0 |
|
|
|
|
|
|
|
|
|
d |
| male 15-24 years SABSSM VI |
50,6 |
|
|
|
|
|
|
|
|
|
d |
| male 25-49 years SABSSM VI |
44,0 |
|
|
|
|
|
|
|
|
|
d |
| male 50+ years SABSSM VI |
27,9 |
|
|
|
|
|
|
|
|
|
d |
| Couple year protection rate |
2022/23 |
DHIS |
45,0 |
41,4 |
83,9 |
28,6 |
58,4 |
46,5 |
43,4 |
38,3 |
48,3 |
50,2 |
b |
| Delivery 10-14 years in facility |
2022/23 |
female 10-14 years DHIS |
3 497 |
553 |
139 |
494 |
794 |
467 |
403 |
81 |
201 |
365 |
b |
| Delivery 10-19 years in facility |
2022/23 |
female 10-19 years DHIS |
132 280 |
17 617 |
6 113 |
20 755 |
34 823 |
17 193 |
12 872 |
3 755 |
8 664 |
10 488 |
b |
| Delivery 15-19 years in facility |
2022 |
15-19 years vital registration |
101 569 |
|
|
|
|
|
|
|
|
|
e |
| 2022/23 |
female 15-19 years DHIS |
128 783 |
17 064 |
5 974 |
20 261 |
34 029 |
16 726 |
12 469 |
3 674 |
8 463 |
10 123 |
b |
| Delivery by Caesarean section rate |
2021 |
NCCEMD |
28,0 |
29,5 |
30,5 |
30,0 |
35,6 |
22,5 |
21,2 |
22,7 |
21,3 |
29,9 |
f |
| 2022/23 |
female DHIS |
31,3 |
33,2 |
34,3 |
32,5 |
36,8 |
25,5 |
23,4 |
26,9 |
25,7 |
32,0 |
b |
| Delivery by Caesarean section rate (district hospitals) |
2022/23 |
female DHIS District Hospital |
27,0 |
26,8 |
14,9 |
33,1 |
30,2 |
25,6 |
22,3 |
16,9 |
33,0 |
28,3 |
b |
| Delivery in 10-19 years in facility rate |
2022/23 |
female DHIS |
13,9 |
17,6 |
13,3 |
9,6 |
16,2 |
14,2 |
16,2 |
17,0 |
14,5 |
11,2 |
b |
| Delivery in facility - total |
2022/23 |
DHIS |
952 141 |
99 915 |
46 076 |
215 111 |
214 511 |
121 057 |
79 685 |
22 047 |
59 869 |
93 870 |
b |
| Early neonatal death in facility rate |
2022/23 |
both sexes DHIS |
9,6 |
10,3 |
11,6 |
9,3 |
9,1 |
10,6 |
10,5 |
11,3 |
10,4 |
7,1 |
b |
| Female condoms distributed |
2022/23 |
DHIS |
15 512 957 |
1 279 500 |
2 182 220 |
4 497 159 |
3 047 100 |
1 071 100 |
1 367 918 |
101 513 |
708 047 |
1 258 400 |
b |
| Live births in facility |
2022/23 |
both sexes DHIS |
947 395 |
99 503 |
46 291 |
214 128 |
212 530 |
120 626 |
79 570 |
22 487 |
59 304 |
92 956 |
b |
| Male condom distribution coverage |
2022/23 |
DHIS |
18,90 |
12,40 |
52,70 |
11,10 |
24,00 |
20,60 |
21,30 |
11,20 |
20,10 |
20,50 |
b |
| Male condoms distributed |
2022/23 |
male DHIS |
402 808 623 |
25 490 700 |
52 469 700 |
69 220 678 |
89 664 600 |
38 910 442 |
35 627 000 |
5 194 000 |
30 810 803 |
55 420 700 |
b |
| Maternal death in facility |
2022/23 |
female DHIS |
1 011 |
133 |
48 |
265 |
176 |
137 |
97 |
20 |
75 |
60 |
b |
| Maternal mortality in facility ratio |
2022/23 |
female DHIS |
101 |
124 |
95 |
119 |
79 |
109 |
115 |
80 |
118 |
62 |
b |
| Mother postnatal visit within 6 days after delivery |
2022/23 |
female DHIS |
761 807 |
80 488 |
36 029 |
168 329 |
168 633 |
118 124 |
60 690 |
14 202 |
58 800 |
56 512 |
b |
| Mother postnatal visit within 6 days rate |
2022/23 |
female DHIS |
80,0 |
80,6 |
78,2 |
78,3 |
78,6 |
97,6 |
76,2 |
64,4 |
98,2 |
60,2 |
b |
| Neonatal death in facility rate |
2022/23 |
both sexes DHIS |
12,7 |
13,8 |
16,2 |
13,2 |
12,0 |
13,1 |
12,9 |
14,2 |
13,4 |
9,0 |
b |
| Stillbirths in facility |
2022/23 |
both sexes DHIS |
20 228 |
2 063 |
1 223 |
4 441 |
5 024 |
2 285 |
1 730 |
499 |
1 277 |
1 686 |
b |
| Stillbirth in facility rate |
2022/23 |
both sexes DHIS |
20,9 |
20,3 |
25,7 |
20,3 |
23,1 |
18,6 |
21,3 |
21,7 |
21,1 |
17,8 |
b |
| Teenage pregnancy |
2022 |
female 14-19 years GHS |
3,80 |
|
|
|
|
|
|
|
|
|
g |
| ToPs (Terminations of Pregnancy) |
2022/23 |
DHIS |
137 998 |
14 741 |
8 166 |
33 481 |
26 200 |
14 926 |
10 004 |
2 279 |
10 160 |
18 041 |
b |
Reference notes
a Antenatal Survey 2022.36
b webDHIS.16
c Thembisa 4.6.69
d HIV Household Survey 2022.35
e Stats SA Live Births 2022.42
f NCCEMD.37
g Stats SA GHS 2022.34
Definitions
• Delivery 10-14 years in facility [Number]: Delivery where the mother is 10-14 years old. These deliveries are done in facilities under the supervision of trained medical/nursing staff.
• Delivery 10-19 years in facility [Number]: Delivery where the mother is 10-19 years old. These deliveries are done in facilities under the supervision of trained medical/nursing staff.
• Delivery 15-19 years in facility [Number]: Delivery where the mother is 15-19 years old. These deliveries are done in facilities under the supervision of trained medical/nursing staff.
• Delivery in facility - total [Number]: Any delivery taking place in a health facility under the supervision of trained medical/nursing staff.
• Female condoms distributed [Number]: Female condoms distributed from a primary distribution site to health facilities or points in the community (e.g. campaigns, non-traditional outlets, etc.).
• Live birth in facility [Number]: Live birth resulting from a delivery in a facility.
• Male condoms distributed [Number]: Male condoms distributed from a primary distribution site to health facilities or points in the community (e.g. campaigns, non-traditional outlets, etc.).
• Maternal death in facility [Number]: Maternal death is death occurring during pregnancy, childbirth and puerperium within 42 days of termination of pregnancy, irrespective of the duration and site of pregnancy and the cause of death (obstetric and non-obstetric).
• Still birth in facility [Number]: Still born infants delivered in a health facility.
• ToPs (Terminations of Pregnancy) [Number]: The number of terminations of pregnancy.
• Antenatal 1st visit before 20 weeks rate [Percentage]: Women who have a booking visit.
• (first visit) before they are 20 weeks (about half way) into their pregnancy as a proportion of all antenatal 1st visits.
• Antenatal 1st visit coverage [Percentage]: The proportion of pregnant women coming for at least one antenatal visit.
• Cervical cancer screening coverage [Percentage of target women]: Cervical smears in women 30 years and older as a proportion of the female population 30 years and older. 80% of these women should be screened for cervical cancer every 10 years and 20% must be screened every 3 years, which should be included in the denominator because it is estimated that 20% of women 30 years and older are HIV positive.
• Condom use at last sex [Percentage]: Percentage of those, who reported ever having had sex, who used a condom the last time they had sex. Note that the precise definition of this indicator varies between surveys.
• Couple year protection rate [Percentage]: Women protected against pregnancy by using modern contraceptive methods, including sterilisations, as proportion of female population 15-49 year. Couple year protection is the total of (Oral pill cycles / 15) + (Medroxyprogesterone injection / 4) + (Norethisterone enanthate injection / 6) + (IUCD x 4.5) + (Sub-dermal implant x 2.5) + Male condoms distributed / 120) + (Female condoms distributed / 120) + (Male sterilisation x 10) + (Female sterilisation x 10).
• Delivery by Caesarean section rate (district hospitals) [Percentage]: Caesarean section deliveries, expressed as the proportion of total deliveries in facility.
• Delivery by Caesarean section rate [Percentage]: Delivery by Caesarean section as proportion of total deliveries in health facilities.
• Delivery in 10 to 19 years in facility rate [Percentage]: Deliveries to women under the age of 20 years as proportion of total deliveries in health facilities.
• Delivery in facility rate [Percentage]: Deliveries in health facilities as proportion of expected deliveries in the population. Expected deliveries are estimated as population under 1 year multiplied by 1.025 to compensate for still births and infant mortality.
• Early neonatal death in facility rate [per 1 000 live births]: Early neonatal deaths per 1000 infants who were born alive in health facilities.
• Male condom distribution coverage [Condoms per male 15+]: Male condoms distributed from a primary distribution site to health facilities or points in the community (e.g. campaigns, non-traditional outlets, etc.).
• Maternal mortality in facility ratio [per 100 000 live births]: Women who die as a result of childbearing, during pregnancy or within 42 days of delivery or termination of pregnancy, per 100 000 live births, and where the death occurs in a health facility.
• Mother postnatal visit within 6 days rate [Percentage]: Mothers who received postnatal care within 6 days after delivery as proportion of deliveries in health facilities.
• Neonatal death in facility rate [per 1 000 live births]: Infants 0-28 days who died during their stay in the facility per 1000 live births in facility.
• Stillbirth in facility rate [per 1 000 births]: Stillbirths in facility per 1 000 total births in a facility.
• Teenage pregnancy [Percentage]: Percentage of women aged 15-19 who are mothers or who have ever been pregnant. The percentage of women who are mothers at the time of the survey is a more restrictive definition. Note that some of the surveys report this indicator as the percentage who have ever been pregnant of those WHO HAVE EVER HAD SEX. This is a different denominator to that used by the Demographic and Health Surveys, and the data can therefore not be directly compared.
Child health
Childhood immunisation coverage
Immunisation represents the most cost-effective child health intervention, as outlined in the Immunisation Agenda 2021-2030.85
South Africa continues to experience unacceptable under-five mortality. In 2022/23, 723 children died from diarrhoea, and 939 from pneumonia. KwaZulu-Natal had the highest diarrhoea and pneumonia deaths, while the Northern Cape had the fewest. The Eastern Cape had the highest diarrhoea case fatality rate, whereas Mpumalanga and Eastern Cape had the highest pneumonia rates, as depicted in Table 8. In 2022 and 2023, the third dose of the pneumococcal conjugate vaccine (PCV) recorded coverage of 89.2% and 84.2%, respectively. Coverage of the second dose of the rotavirus vaccine (RV) in the same years was 83.5% and 77.6%, respectively. Vaccine coverage for both antigens was therefore lower than in the previous year, as shown in Figure 21. National or provincial coverage percentages can hide other disparities, such as delays in immunisation scheduling. Four Western Cape public sector facilities found that coverage fell from birth to 18 months, with the third diphtheria-tetanus-pertussis (DTP) vaccination dose delayed the most (defined as receiving immunisations more than 28 days after the recommended schedule age).86 Lower socioeconomic status and upper-middle socioeconomic status were risk factors for delayed or skipped immunisation, possibly due to work demands.87

Figure 20.Pneumococcal conjugate vaccine and rotavirus vaccine 3rd dose coverage, 2021-2023
As an indicator of the efficacy of routine immunisation services for children, the WHO recommends that countries achieve a minimum of 90% coverage for the third dose of diphtheria-tetanus-pertussis (DTP3).28 South Africa’s immunisation coverage is still below optimal levels, not only for DTP3, but also for all age-specific immunisations. Additional age-specific immunisation data are documented in Table 8 and Figure 22.
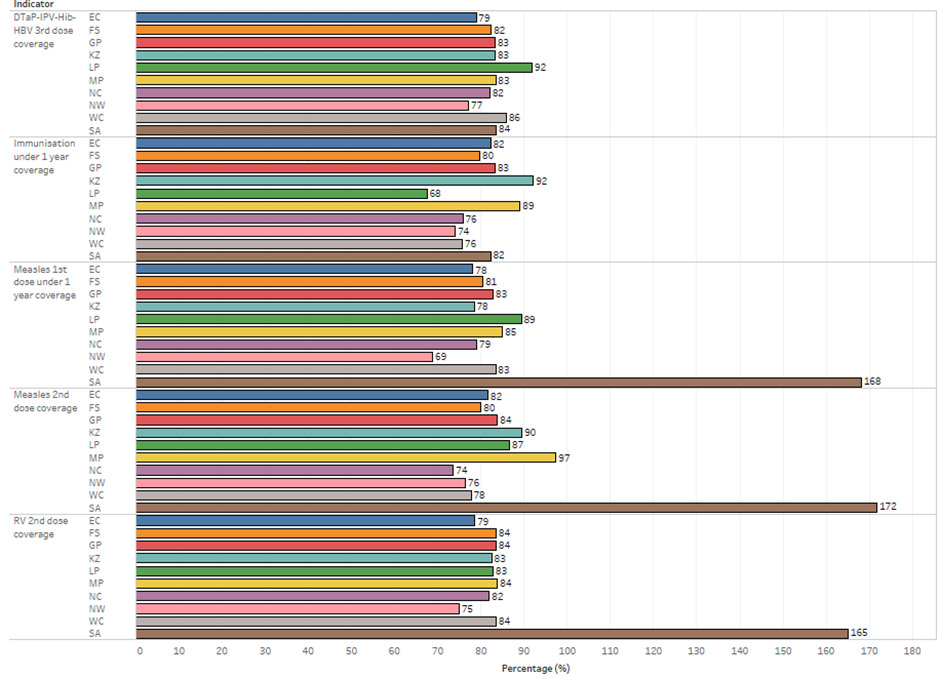
Figure 21.Childhood immunisation coverage by provinces, 2022/23
Vaccine preventable disease outbreaks
It is crucial to achieve optimal coverage in childhood immunisation to prevent disease outbreaks and ensure community immunity.88 A situation report regarding a measles outbreak was published by the NICD on 26 January 2023. The report confirmed 421 laboratory-diagnosed cases from epidemiological week 40 of 2022 to the middle of week 3 of 2023. In provinces that were affected by outbreaks, the 5-9-year-old age group comprised the majority of cases (160/406, 39%). The under-1-year age group accounted for the highest proportion of cases, with 15/27 (59%), originating from hospitals rather than primary health care clinics. Nevertheless, the age group of 10-14-years continued to experience cases (64/406,16%), underscoring the importance of including this demographic in a vaccination campaign.88
Similarly, a rise in laboratory-confirmed pertussis cases from the pneumonia surveillance programme was seen in 2022/3, particularly in the Western Cape, Mpumalanga, Gauteng, KwaZulu-Natal, and North West, as depicted in Figure 23.89 The NICD received 818 pertussis case reports from 1 January 2022 to 19 January 2023, with 95.8% (784/818) occurring between July 2022 and January 2023. The Western Cape reported 60.2% (472/784) of the 784 cases. The majority (58.0%, 455/784) of reported cases were in children under five, with 78.0% (355/455) under three months old.89

Figure 22.Number of laboratory-confirmed pertussis cases form pneumonia surveillance programme by year, month, and province, 2018-2023
Source: NICD Communique, January 2023.72
A recent study found a link between health expenditures (as a percentage of gross domestic product (GDP)) and vaccination coverage for Bacillus Calmette-Guerin (BCG) and DTP3 in sub-Saharan Africa.90 This highlights the significance of proper funding for vaccination programmes in order to achieve high coverage rates. The District Health Service programme spent a total of R2 348 per capita on vaccines per population under one year during 2022/23 (Figure 24). All provinces spent an average of R2 079 per capita on children under the age of one, with Limpopo and KwaZulu-Natal spending the most and Northern Cape and North West spending the least.21

Figure 23.Vaccine expenditure by province, 2022/23
Table 8.Child health indicators by province
| Indicator |
Period |
Sex|Age|Series|Cat |
SA |
EC |
FS |
GP |
KZ |
LP |
MP |
NC |
NW |
WC |
Ref |
| BCG coverage |
2022 |
both sexes WHO/UNICEF |
84,0 |
|
|
|
|
|
|
|
|
|
a |
| Child mortality (deaths between 1-4 years per 1 000 live births) |
2021 |
both sexes WHO |
32,9 |
|
|
|
|
|
|
|
|
|
b |
| female WHO |
30,3 |
|
|
|
|
|
|
|
|
|
b |
| male WHO |
35,3 |
|
|
|
|
|
|
|
|
|
b |
| Child under 5 years pneumonia incidence |
2022/23 |
both sexes DHIS |
25,1 |
13,0 |
26,3 |
19,4 |
19,7 |
13,0 |
6,4 |
14,2 |
5,2 |
110,9 |
c |
| Death in facility under 1 year |
2022/23 |
both sexes DHIS |
15 523 |
1 867 |
961 |
3 514 |
3 319 |
2 040 |
1 314 |
420 |
1 011 |
1 077 |
c |
| Death in facility under 5 years |
2022/23 |
both sexes DHIS |
17 515 |
2 095 |
1 096 |
3 972 |
3 738 |
2 352 |
1 438 |
492 |
1 148 |
1 184 |
c |
| Diarrhoea case fatality under 5 years rate |
2022/23 |
both sexes DHIS |
1,7 |
2,6 |
1,8 |
1,9 |
1,8 |
2,0 |
2,2 |
1,5 |
1,3 |
0,3 |
c |
| Diarrhoea death under 5 years |
2022/23 |
both sexes DHIS |
723 |
119 |
36 |
130 |
184 |
118 |
68 |
17 |
30 |
21 |
c |
| Diarrhoea separation under 5 years |
2022/23 |
both sexes DHIS |
42 586 |
4 539 |
1 979 |
7 023 |
10 170 |
5 815 |
3 036 |
1 161 |
2 353 |
6 510 |
c |
| DTaP-IPV-Hib-HBV 3rd dose coverage |
2022/23 |
both sexes DHIS |
83,50 |
78,90 |
82,40 |
83,30 |
83,20 |
91,90 |
83,40 |
82,10 |
77,10 |
85,90 |
c |
| DTaP-IPV-Hib-HBV (Hexavalent) 3rd dose |
2022/23 |
both sexes DHIS |
948 068 |
103 563 |
41 479 |
218 329 |
211 236 |
115 192 |
79 317 |
20 753 |
62 168 |
96 031 |
c |
| DTP3 coverage |
2022 |
both sexes WHO/UNICEF |
85 |
|
|
|
|
|
|
|
|
|
a |
| Immunisation under 1 year coverage |
2022/23 |
both sexes DHIS |
82,20 |
82,30 |
79,70 |
83,20 |
92,20 |
67,50 |
89,10 |
75,90 |
74,10 |
75,70 |
c |
| Measles 1st dose under 1 year coverage |
2022 |
both sexes WHO |
87,00 |
|
|
|
|
|
|
|
|
|
b |
| 2022/23 |
both sexes DHIS |
81,10 |
78,20 |
80,50 |
82,90 |
78,40 |
89,40 |
85,00 |
79,00 |
68,80 |
83,40 |
c |
| Measles 2nd dose coverage |
2022 |
both sexes WHO/UNICEF |
87,00 |
|
|
|
|
|
|
|
|
|
a |
| 2022/23 |
both sexes DHIS |
84,80 |
81,70 |
80,00 |
83,90 |
89,50 |
86,60 |
97,40 |
73,60 |
76,40 |
77,70 |
c |
| Number of orphans |
2022 |
0-17 years GHS Double orphaned |
497 000 |
85 000 |
27 000 |
97 000 |
120 000 |
51 000 |
30 000 |
10 000 |
40 000 |
37 000 |
d |
| Number of under-5 deaths |
2021 |
both sexes WHO |
38 868 |
|
|
|
|
|
|
|
|
|
b |
| both sexes WHO/UNICEF |
39 000 |
|
|
|
|
|
|
|
|
|
e |
| female WHO |
17 556 |
|
|
|
|
|
|
|
|
|
b |
| male WHO |
21 312 |
|
|
|
|
|
|
|
|
|
b |
| Orphanhood |
2022 |
both sexes <18 years Census double |
2,5 |
3,4 |
3,1 |
2,1 |
2,8 |
2,4 |
2,6 |
2,4 |
2,9 |
1,5 |
f |
| both sexes <18 years Census maternal |
2,3 |
2,8 |
2,8 |
1,9 |
2,5 |
1,8 |
2,5 |
3,1 |
2,6 |
1,6 |
f |
| both sexes <18 years Census paternal |
8,9 |
11,5 |
10,3 |
7,4 |
10,4 |
8,6 |
8,6 |
7,8 |
8,7 |
6,1 |
f |
| both sexes <18 years GHS double |
2,1 |
2,9 |
2,4 |
1,9 |
2,4 |
1,7 |
1,6 |
1,8 |
2,4 |
1,5 |
d |
| both sexes <18 years GHS maternal |
2,5 |
2,7 |
3,9 |
2,3 |
2,3 |
2,3 |
2,7 |
3,2 |
2,7 |
1,7 |
d |
| both sexes <18 years GHS paternal |
7,7 |
8,7 |
9,8 |
7,0 |
8,9 |
6,7 |
8,3 |
5,5 |
8,6 |
5,4 |
d |
| PCV 3rd dose coverage |
2021 |
|
87 |
|
|
|
|
|
|
|
|
|
g |
| PCV 3rd dose coverage |
2022 |
both sexes WHO/UNICEF |
85 |
|
|
|
|
|
|
|
|
|
a |
| Pneumonia case fatality under 5 years rate |
2022/23 |
both sexes <5 years DHIS |
1,50 |
2,80 |
1,70 |
1,50 |
1,90 |
2,60 |
2,80 |
2,40 |
1,40 |
0,24 |
c |
| Pneumonia death under 5 years |
2022/23 |
both sexes DHIS |
939 |
139 |
46 |
168 |
220 |
161 |
99 |
26 |
40 |
40 |
c |
| RV 2nd dose coverage |
2022 |
both sexes WHO/UNICEF |
83,00 |
|
|
|
|
|
|
|
|
|
a |
| 2022/23 |
both sexes DHIS |
82,1 |
78,6 |
83,5 |
83,6 |
82,6 |
82,9 |
83,8 |
81,9 |
74,9 |
83,5 |
c |
| School Grade 1 screening coverage |
2022/23 |
both sexes DHIS |
21,2 |
4,9 |
23,4 |
30,2 |
21,8 |
11,3 |
22,1 |
14,3 |
27,4 |
35,0 |
c |
| School Grade 8 screening coverage |
2022/23 |
both sexes DHIS |
14,5 |
1,5 |
19,9 |
28,8 |
13,2 |
10,1 |
11,0 |
3,6 |
21,7 |
9,6 |
c |
| Severe acute malnutrition case fatality under 5 years rate |
2022/23 |
both sexes DHIS |
7,2 |
7,6 |
9,7 |
6,5 |
9,2 |
7,4 |
7,8 |
8,5 |
3,9 |
2,4 |
c |
| Severe acute malnutrition death under 5 years |
2022/23 |
both sexes DHIS |
836 |
98 |
98 |
129 |
206 |
129 |
54 |
52 |
56 |
14 |
c |
| Under 5 mortality rate |
2021 |
both sexes WHO/UNICEF |
33,00 |
|
|
|
|
|
|
|
|
|
e |
| Vaccine expenditure per population under 1 year |
2022/23 |
all programs real 2022/23 prices |
2 544 |
2 304 |
2 588 |
2 409 |
2 655 |
3 911 |
2 326 |
16 |
2 933 |
1 813 |
h |
| PR2 real 2022/23 prices |
2 348 |
2 290 |
2 547 |
2 405 |
2 587 |
3 911 |
2 242 |
480 |
481 |
1 764 |
h |
Reference notes
a Immunisation 2022.30
b Global Health Observatory, 2024.91
c webDHIS.16
d Stats SA GHS 2022.34
e State of the world’s children 2023.28
f Census 2022.34
g World Health Statistics 2023.24
h DHB 2022/23.21
Definitions
• Death in facility under 1 year [Number].
• Death in facility under 5 years [Number].
• Number of orphans [Number]: Number of children under 18 years whose biological mother, biological father or both parents have died. Different kinds of orphans are defined as: maternal orphans - a child whose mother has died, or whose living status is not known, but whose father is alive. paternal orphans - a child whose father has died, or whose living status is not known, but whose mother is alive. double/dual orphan - a child whose mother and father have both died, or whereabouts are unknown.
• Number of under-5 deaths [Number]: The estimated number of deaths in children younger than 5 years.
• Pneumonia death under 5 years [Number]: A child under 5 years who died in a health facility where pneumonia was documented as the main cause of death.
• Severe acute malnutrition death under 5 years [Number]: Death in child under 5 years with severe acute malnutrition (SAM).
• BCG coverage [Percentage]: The proportion of expected live born babies that received BCG under 1 year of age (note: usually given immediately after birth).
• Child under 5 years pneumonia incidence [Cases per 1 000 children]: Children under 5 years newly diagnosed with pneumonia per 1 000 children under 5 years in the population.
• Child under 5 years severe acute malnutrition incidence [Cases per 1 000 children]: Children under 5 years newly diagnosed with severe acute malnutrition per 1 000 children under 5 years in the population.
• Diarrhoea case fatality under 5 years rate [Percentage]: Diarrhoea deaths in children under 5 years as a proportion of diarrhoea separations under 5 years in health facilities.
• Diarrhoea incidence under 5 years [Cases per 1 000 children]: Children with diarrhoea per 1 000 children in the catchment population. Diarrhoea is formally defined as 3 or more watery stools in 24 hours, but any episode diagnosed and/or treated as diarrhoea after an interview with the adult accompanying the child.
• DTaP-IPV-Hib-HBV 3rd dose coverage [Percentage]: Children under 1 year who received DTaP-IPV-Hib-HBV 3rd dose, normally at 14 weeks as a proportion of population under 1 year. Both Pentaxim and Hexavalent will form part of the numerator to ensure accurate coverage of historical data.
• DTaP-IPV-Hib-HBV 4th dose coverage [Percentage]: Children under 2 years who received DTaP-IPV-Hib-HBV 4th dose, normally at 18 months as a proportion of the 1 year population. Both Pentaxim and Hexavalent will form part of the numerator to ensure accurate coverage of historical data.
• DTP3 coverage [Percentage]: The proportion of children who received their third DTP doses (normally at 14 weeks).
• Immunisation under 1 year coverage [Percentage]: The proportion of all children in the target area under one year who complete their primary course of immunisation. A primary course includes BCG, OPV 1,2 & 3, DTP-Hib 1,2 & 3, HepB 1,2 & 3, and 1st measles (usually at 9 months).
• Infant mortality rate (deaths under 1 year per 1 000 live births) [per 1 000 live births]: The number of children less than one year old who die in a year, per 1 000 live births during that year.
• Measles 1st dose under 1 year coverage [Percentage]: Children under 1 year who received measles 1st dose, as a proportion of population under 1 year.
• Measles 2nd dose coverage [Percentage]: Children 1 year (12 months) who received measles 2nd dose, as a proportion of the 1-year population.
• Orphanhood [Percentage]: Proportion of children under 18 years whose biological mother, biological father or both parents have died.
• PCV 3rd dose coverage [Percentage]: Children under 1 year who received PCV 3rd dose, normally at 9 months as a proportion of population under 1 year.
• Pneumonia case fatality under 5 years rate [Percentage]: Pneumonia deaths in children under 5 years as a proportion of pneumonia separations under 5 years in health facilities.
• Pneumonia case survival under 5 years rate [Scale 0-100]: The smoothed estimates of the pneumonia CFR were generated from the webDHIS indicator using a generalised additive model with thin-plate splines, after removing outlier values. The smoothed CFR was then rescaled according to the maximum observed value according to the formula: index = (max CFR - CFR) / (max CFR - min CFR)*100. This rescaled value thus represents a survival rate (the inverse of the case fatality rate).
• RV 2nd dose coverage [Percentage]: Children under 1 year who received RV 2nd dose as a proportion of children under 1 year.
• School Grade 1 screening coverage [Percentage]: Proportion of Grade 1 learners screened by a nurse in line with the ISHP service package.
• School Grade 8 screening coverage [Percentage]: Proportion of Grade 8 learners screened by a nurse in line with the ISHP service package.
• Severe acute malnutrition case fatality under 5 years rate [Percentage]: Severe acute malnutrition deaths in children under 5 years as a proportion of severe acute malnutrition (SAM) under 5 years in health facilities.
• Under 5 mortality rate (deaths under 5 years per 1 000 live births) [per 1 000 live births]: The number of children under 5 years who die in a year, per 1 000 live births during the year. It is a combination of the infant mortality rate, plus the age 1-4 mortality rate.
• Vaccine expenditure per population under 1 year [Rand per population U1 (real prices)]: Provincial expenditure on vaccines per population under 1 year.
Non-communicable diseases
Globally, the World Health Statistics 2023 has noted that the “epidemic of NCDs poses devastating health consequences for individuals, families and communities”.24(p10) The four major NCDs (cardiovascular disease, cancer, chronic respiratory disease, and diabetes) were collectively responsible for 33.3 million (uncertainty interval (UI): 24.5 – 43.3 million) deaths in 2019, representing a 28% increase compared to 2000. However, the increase in absolute numbers of deaths due to NCDs was driven mainly by population growth and ageing. Age-standardised mortality rates have been declining for the main NCDs, other than diabetes. In 2021, the Global Burden of Disease (GBD) study estimated that there were 529 million people living with diabetes worldwide, of which 96.0% were living with type 2 diabetes.92 Based on data from 44 low- and middle-income countries, poor access was shown to four diabetes prevention activities (physical activity counselling, weight loss counselling, dietary counselling, and blood glucose screening).93
The consequences of poor NCD care were laid bare in the Stats SA report entitled Non-communicable diseases in South Africa: Findings from death notifications 2008–2018, published in 2023.94 The report showed that deaths attributable to NCDs increased by 58.7% over 20 years, from 103 428 in 1997 to 164 205 in 2018, possibly due to population increases. For diabetes in particular, the age-standardised mortality rates (ASMR) increased from 58.5 per 100 000 in 2008 to 62.9 per 100 000 in 2018. The diabetes ASMR for females was higher in 2018 (64.3 per 100 000) than for males (60.3 per 100 000). The report noted that “recommendations for a comprehensive surveillance and monitoring system for NCDs need to be implemented to establish baselines and monitor the 90-60-50 target cascade for non-communicable diseases”.94(piv)
As shown in Table 9, with the webDHIS reports on diabetes screening rates, there are no measures of diabetes control. Based on a large cohort of 373 889 patients tested for either glycosylated haemoglobin (HbA1c) or blood glucose by the National Health Laboratory Service (NHLS) over a 27-month period (January 2012 to March 2015), it was estimated that only 30.9% of those diagnosed with diabetes were retained in care and only 8.7% achieved glycaemic control.95 Prevalence data reported by the Council for Medical Schemes, based on claims data, also cannot provide any information on effective treatment coverage.
In stark contrast to the plethora of indicators available to track diagnosis, treatment, and outcomes related to infectious diseases, routine data on NCDs remains sparse. This is despite the commitment in the National Strategic Plan for the Prevention and Control of Non-Communicable Diseases 2022-2027 to 90-60-50 cascade states, where 90% of all people over 18 will know whether or not they have raised blood pressure and/or raised blood glucose, 60% of people with raised blood pressure or blood glucose will receive intervention, and 50% of people receiving such interventions will be controlled.96
Commenting on the monitoring and evaluation system used to measure the performance of primary healthcare delivered through the district health system in South Africa, Barron et al. pointed to “a general lack of patient-centred and community responsiveness indicators”.97(p1519) The authors identified a mismatch between the number of indicators in the National Indicator Data Set (NIDS) and the importance attached to each category of indicators. While there were 70 indicators for the HIV programme, for instance, there were only 6 indicators for all NCDs.
Despite the National Strategic Plan’s ambitious goals, challenges in data collection and evaluation persist, especially in tracking patient outcomes and ensuring effective treatment. The increasing burden of NCDs, as evidenced by rising mortality rates and poor disease control, underscores the urgent need for comprehensive surveillance systems. The available NCD indicators are shown in Table 9.
Table 9.Non-communicable disease indicators by province
| Indicator |
Period |
Sex|Age|Series|Cat |
SA |
EC |
FS |
GP |
KZ |
LP |
MP |
NC |
NW |
WC |
Ref |
| Client 18-44 years screened for diabetes |
2022/23 |
both sexes DHIS |
24 275 066 |
3 129 155 |
781 624 |
4 670 049 |
9 016 732 |
2 908 590 |
2 122 397 |
268 403 |
1 378 116 |
|
a |
| Dental utilisation rate |
2022/23 |
both sexes all ages DHIS |
39,8 |
43,5 |
40,4 |
46,7 |
48,2 |
7,3 |
31,3 |
34,2 |
21,4 |
52,0 |
a |
| Diabetes client treatment new 45 years and older |
2022/23 |
DHIS |
0,6 |
0,7 |
0,2 |
0,5 |
0,4 |
1,8 |
1,1 |
0,8 |
0,5 |
0,1 |
a |
| Diabetes prevalence (per 1 000) |
2021 |
both sexes all ages med schemes Diabetes mellitus Type 1 |
3,0 |
|
|
|
|
|
|
|
|
|
b |
| both sexes all ages med schemes Diabetes mellitus Type 2 |
57,9 |
|
|
|
|
|
|
|
|
|
b |
| 2022 |
both sexes all ages med schemes Diabetes mellitus Type 1 |
4,8 |
|
|
|
|
|
|
|
|
|
b |
| both sexes all ages med schemes Diabetes mellitus Type 2 |
60,1 |
|
|
|
|
|
|
|
|
|
b |
| Hyperlipidaemia prevalence (per 1 000) |
2021 |
both sexes med schemes all beneficiaries |
69,9 |
|
|
|
|
|
|
|
|
|
b |
| female med schemes all beneficiaries |
41,6 |
|
|
|
|
|
|
|
|
|
b |
| male med schemes all beneficiaries |
52,3 |
|
|
|
|
|
|
|
|
|
b |
| 2022 |
both sexes med schemes all beneficiaries |
73,2 |
|
|
|
|
|
|
|
|
|
b |
| female med schemes all beneficiaries |
44,2 |
|
|
|
|
|
|
|
|
|
b |
| male med schemes all beneficiaries |
54,0 |
|
|
|
|
|
|
|
|
|
b |
| Hypertension prevalence (per 1 000) |
2021 |
both sexes med schemes all beneficiaries |
157,6 |
|
|
|
|
|
|
|
|
|
b |
| female med schemes all beneficiaries |
110,5 |
|
|
|
|
|
|
|
|
|
b |
| male med schemes all beneficiaries |
98,9 |
|
|
|
|
|
|
|
|
|
b |
| 2022 |
both sexes med schemes all beneficiaries |
159,8 |
|
|
|
|
|
|
|
|
|
b |
| female med schemes all beneficiaries |
112,3 |
|
|
|
|
|
|
|
|
|
b |
| male med schemes all beneficiaries |
99,9 |
|
|
|
|
|
|
|
|
|
b |
| Mental disorders treatment rate new |
2022/23 |
DHIS |
0,1 |
0,1 |
0,0 |
0,1 |
0,1 |
0,2 |
0,0 |
0,1 |
0,0 |
|
a |
| Mental health separation rate |
2022/23 |
DHIS |
3,7 |
2,5 |
17,0 |
2,3 |
2,2 |
2,2 |
1,8 |
1,1 |
1,7 |
4,4 |
a |
| Prevalence of non-raised blood pressure |
2019 |
both sexes 30-79 years WHO age-standardised |
23,6 |
|
|
|
|
|
|
|
|
|
c |
| both sexes 30-79 years WHO crude |
22,0 |
|
|
|
|
|
|
|
|
|
c |
| female 30-79 years WHO age-standardised |
29,9 |
|
|
|
|
|
|
|
|
|
c |
| female 30-79 years WHO crude |
29,0 |
|
|
|
|
|
|
|
|
|
c |
| male 30-79 years WHO age-standardised |
16,4 |
|
|
|
|
|
|
|
|
|
c |
| male 30-79 years WHO crude |
14,2 |
|
|
|
|
|
|
|
|
|
c |
Reference notes
a webDHIS.16
b Medical schemes 2022.48
c Global Health Observatory, 2024.98
Definitions
• Client 18-44 years screened for diabetes [Number]: Client 18 - 44 years, not on treatment for diabetes, screened for diabetes in the facility.
• Dental utilisation rate [per 1000 population]: Dental visits per 1000 uninsured population.
• Diabetes prevalence (per 1 000) [per 1 000 population]: Number of people with diabetes per 1 000 people in the target population.
• Diabetes prevalence [Percentage]: Percentage of people with diabetes. Defined in SANHANES as those with HbA1c > 6.5%. WHO Core indicator is: Age-standardised prevalence of raised blood glucose/diabetes among persons aged 18+ years or on medication for raised blood glucose Defined as: fasting plasma glucose value >= 7.0 mmol/L (126 mg/dL) or on medication for raised blood glucose among adults aged 18+ years."
• Hyperlipidaemia prevalence (per 1 000) [per 1 000 population]: Number of people with hyperlipidaemia per 1 000 people in the target population. Data for the private sector are based on the number of people being TREATED for this condition.
• Hypertension prevalence (per 1 000) [per 1 000 population]: Number of people with hypertension.
• Mental disorders treatment rate new [Percentage]: Clients treated for mental disorders (depression, anxiety, dementia, psychosis, mania, suicide, developmental disorders, behavioural disorders and substance use) as a proportion of total PHC headcount.
• Mental health separation rate [Percentage]: Proportion of clients admitted for mental health problems. Inpatient separations are the total of inpatient discharges, inpatient deaths and inpatient transfers out.
• Prevalence of non-raised blood pressure [Percentage]: The prevalence of normal blood pressure, regardless of treatment status, is the sum of those who do not have hypertension and those whose hypertension is controlled by medication.
Injuries and risk behaviours
Road and pedestrian safety
Annually, the Road Traffic Management Corporation (RTMC) reports on the state of road safety, covering a 12-month period. The RTMC states that, nationally, road accident fatalities have decreased from 12 541 in 2021 to 12 436 in 2022. As expected, Gauteng reported the highest and Northern Cape the lowest number of fatalities. In addition, the fatality rate per 100 000 people decreased slightly from 20.7 in 2021 to 20.5 in 2022. Many of these fatalities were among pedestrians, followed by passengers, drivers and cyclists, in both 2021 and 2022.99
Drug abuse
The South African Community Epidemiology Network on Drug Use (SACENDU) gathers information from individuals who use drugs (PWUD), including those who inject drugs (PWID). According to the SACENDU Phase 54 policy brief, data from the first half of 2023 (January-June 2023) shows that there were 11 563 admissions for alcohol and other drug abuse across all age groups and sexes. This represents a decrease from 11 923 in the first half of 2022 (January to June 2022) and an increase when compared to 10 170 in the second half of 2022 (July to December 2022).47,100 Primary drugs of abuse are presented in Table 10 along with the prevalence of smoking among both sexes aged 15 years and older.
Gender-based violence
Statistics on gender-based violence (GBV) in South Africa are available, although there are substantial gaps and limitations in data collection and reporting.101 The country’s statistics are compiled from a variety of sources, including police records, health services, and non-governmental organisations. However, these sources frequently present an incomplete picture due to underreporting, stigma, and a lack of comprehensive national data systems. In 2020, Stats SA released a report of an analysis of the phenomenon of GBV and femicide using data from the 2018/19 Governance, Public Safety and Justice Survey.101 It was reported that about 50% of assaults were committed by persons known to the victim. That is, 22% were friends/acquaintances, 15.2% were spouses or intimate partner, and 12.6% were relatives/other household member of the female victims. In addition, when stratified by marital status, it was found that divorced or separated women were more likely to experience physical (40%) and sexual violence (16%), than those living together (physical: 31%; sexual: 10%), widowed (physical: 24%, sexual: 8%), never married (physical: 18%, sexual: 5%), and married (physical: 14%, sexual: 4%).
Intentional and unintentional injuries
The South African Medical Council’s Burden of Disease Unit conducted three nationally representative injury mortality (IM) and causes surveys in 2009, 2017, and 2020/21. Non-natural deaths are defined in these studies as homicides, suicides, and other unintentional harm deaths. The anticipated national age-standardised injury rate was reported to be 109, 95.3, and 89.9 per 100 000 people in 2009, 2017, and 2020/21, respectively, indicating a decline in any injury-related death over time.102,103
Homicide
Between 2009 and 2021, the rate of homicide decreased from 38.4 to an adjusted 37.1 and 37 per 100 000 population, respectively, over the course of three years. In 2009, the number of firearm homicides increased from 11.2 to an amended 12.0, and then to 16.0 in 2020/21. The homicide rates of males were consistently higher than those of females in all reports.102,103
The age-standardised suicide mortality rate fell from 13.4 (95% CI: 11.6-15.2) in 2000 to 12.1 in 2017 and 11.5 in 2020-21. The age-standardised rates of other unintentional injury deaths have risen in the last three years. The age-standardised injury fatality rates increased by 25.9% between 2009 and 2017, and by 12.4% between 2017 and 2020/21.103
The IM surveys show that homicide and suicide rates are declining over time. This suggests that other unintended injuries should be monitored more rigorously. Annual nationally representative surveys are required to better document the number of deaths from violence and injury. Due to the scarcity of current statistics, covering other causes of death such as femicide, interpersonal violence, and GBV will be beneficial.
Table 10.Injuries and risk indicators by province
| Indicator |
Period |
Sex|Age|Series|Cat |
SA |
EC |
FS |
GP |
KZ |
LP |
MP |
NC |
NW |
WC |
Ref |
| Road accident fatalities |
2021 |
both sexes all ages RTMC |
12 541 |
1 533 |
799 |
2 557 |
2 409 |
1 400 |
1 261 |
403 |
908 |
1 271 |
a |
| 2022 |
both sexes all ages RTMC |
12 436 |
1 471 |
740 |
2 561 |
2 308 |
1 376 |
1 293 |
417 |
832 |
1 438 |
a |
| Road accident fatalities per 100 000 population |
2019 |
both sexes Stats SA |
11,0 |
15,2 |
10,1 |
2,5 |
14,7 |
22,9 |
10,1 |
32,4 |
14,6 |
7,2 |
b |
| female Stats SA |
5,4 |
|
|
|
|
|
|
|
|
|
b |
| male Stats SA |
17,1 |
|
|
|
|
|
|
|
|
|
b |
| Number of admissions for alcohol and other drug abuse |
Jan-Jun 2023 |
both sexes all ages SACENDU |
11 563 |
247 |
|
7 550 |
1 062 |
|
|
|
|
1 685 |
c |
| Prevalence of smoking |
2022 |
both sexes 15 years and older WHO |
20,3 |
|
|
|
|
|
|
|
|
|
d |
| Prevalence of smoking |
female 15 years and older WHO |
6,5 |
|
|
|
|
|
|
|
|
|
d |
| Prevalence of smoking |
male 15 years and older WHO |
35,1 |
|
|
|
|
|
|
|
|
|
d |
| Primary drug of abuse as % of all drugs of abuse |
Jan-Jun 2023 |
both sexes <19 years SACENDU alcohol |
|
9,0 |
|
5,0 |
4,0 |
|
|
|
|
11,0 |
c |
| both sexes <19 years SACENDU cannabis |
|
71,0 |
|
79,0 |
75,0 |
|
|
|
|
81,0 |
c |
| both sexes <19 years SACENDU cocaine |
|
2,0 |
|
0,0 |
1,0 |
|
|
|
|
1,0 |
c |
| both sexes <19 years SACENDU heroin |
|
0,0 |
|
0,0 |
1,0 |
|
|
|
|
0,0 |
c |
| both sexes <19 years SACENDU mandrax |
|
0,0 |
|
2,0 |
4,0 |
|
|
|
|
1,0 |
c |
| both sexes <19 years SACENDU methamphethamine |
|
15,0 |
|
7,0 |
0,0 |
|
|
|
|
4,0 |
c |
| both sexes all ages SACENDU alcohol |
28,0 |
34,0 |
|
12,0 |
36,0 |
|
|
|
|
19,0 |
c |
| both sexes all ages SACENDU cannabis |
55,0 |
29,0 |
|
34,0 |
28,0 |
|
|
|
|
23,0 |
c |
| both sexes all ages SACENDU cocaine |
11,0 |
3,0 |
|
2,0 |
11,0 |
|
|
|
|
2,0 |
c |
| both sexes all ages SACENDU heroin |
24,0 |
1,0 |
|
17,0 |
14,0 |
|
|
|
|
17,0 |
c |
| both sexes all ages SACENDU mandrax |
20,0 |
3,0 |
|
3,0 |
2,0 |
|
|
|
|
6,0 |
c |
| both sexes all ages SACENDU methamphethamine |
41,0 |
23,0 |
|
24,0 |
3,0 |
|
|
|
|
31,0 |
c |
| Total alcohol per capita (age 15+ years) consumption (litres per year) |
2019 |
|
8,8 |
|
|
|
|
|
|
|
|
|
e |
Reference notes
a Road safety report 2022.99
b Stats SA Road Accident Deaths.40
c SACENDU Phase 54.100
d WHO Global Estimate.31
e World Health Statistics 2023.24
Definitions
• Road accident fatalities - No]: Number of people killed during or immediately after a crash, or death within 30 days after a crash happened as a direct result of such crash.
• Road accident fatalities per 100 000 population - per 100 000 population]: Number of fatalities due to road accidents per 100 000 population. WHO Core indicator is Mortality rate from road traffic injuries (per 100 000 population) Defined as: Number of road traffic fatal injury deaths per 100 000 population (age-standardised).
• Number of admissions for alcohol and other drug abuse - Number]: Number of patients admitted for treatment by treatment centres who are part of the SACENDU Project sentinel surveillance system. Where data for the latter 3 have not been disaggregated these are included in the national total.
• Prevalence of smoking - Percentage]: Proportion of population who currently smoke. This indicator is also known as 'Current smokers (%)’. Note that the indicator may be given just for cigarettes or for other tobacco products. The WHO Core indicator is ‘Age-standardised prevalence of current tobacco use among persons aged 18+ years’ and is defined as: Age-standardised prevalence of current tobacco use among persons aged 18+ years. “Smoked tobacco products” include the consumption of cigarettes, bidis, cigars, cheroots, pipes, shisha (water pipes), fine-cut smoking articles (roll-your-own), krekets, and any other form of smoked tobacco.
• Primary drug of abuse as % of all drugs of abuse - Percentage]: Percentage breakdown of the primary drug of abuse reported by patients admitted to treatment centres that are part of the SACENDU sentinel surveillance system.
• Total alcohol per capita (age 15+ years) consumption (litres per year) - litres per person]: Total alcohol per capita is the total amount (sum of recorded alcohol per capita three-year average and unrecorded alcohol per capita) of alcohol consumed per adult (15+ years) in a calendar year, in litres of pure alcohol.
Health services indicators
Health facilities
Health facility indicators are crucial metrics that provide insight into the performance of and challenges faced by healthcare services in South Africa. These indicators include the inpatient crude death rates, bed utilisation rates, primary healthcare (PHC) utilisation rates, and Universal Health Coverage (UHC) index.
Inpatient crude death rate
The crude mortality rate of inpatients is a critical health facility indicator that quantifies the percentage of patients who demise during their admission to a healthcare facility within a specified time frame. This rate offers a variety of critical insights into the healthcare system, including the quality of care, the severity of illness, the impact of epidemics and pandemics, and appropriate resource allocation. The inpatient crude death rate in South Africa was 4.6% in 2022/23, a decrease from the peak of the COVID-19 pandemic at 5.7%, as shown in Table 11.
Primary healthcare and bed utilisation rates
Nationally, the bed utilisation rate increased from 60.7% in 2022 to 66.9% in 2023. This increase indicates that more patients were discharged after being admitted, reflecting an improvement in hospital turnover rates and possibly in patient care efficiency.
The PHC utilisation rate was higher among children under five years old compared to the general population. This could be due to the fact that under-five-year-olds require more frequent encounters at primary care level, such as immunisation visits.
The number of clients seen by professional nurses and doctors has decreased over time, from 120 million in 2019 to 101 393 994 in 2022. This figure marginally increased to 106 401 284 in 2023. There are a number of possible reasons that could be contributing to the decreased PHC headcount, including higher utilisation of the chronic medicine decentralisation programmes, changes in health-seeking behaviours, and significant increases in home visits by community-based services. Nevertheless, KwaZulu-Natal and Gauteng reported a higher number of patients seen by professional nurses or doctors, which may indicate regional disparities in healthcare access.
UHC index and coverage of essential health services
The Universal Health Coverage (UHC) index for 2023 assigned South Africa’s health system a score of 51.6, reflecting significant challenges in the provision of essential, effective health services across the population. This score, derived from the Global Burden of Disease (GBD) 2016 scale, underscores the gaps in service coverage that persist within the country’s health system. These deficiencies indicate that South Africa is not on track to achieve the targets set by Sustainable Development Goal (SDG) 3.8, which aims to ensure universal access to quality health services and financial protection.104
However, the calculation of the UHC index is not without its challenges, particularly in the context of limited data availability on NCDs. Scarcity of reliable data on the prevalence, treatment, and outcomes of NCDs complicates the assessment of service coverage and effectiveness. This data gap may result in an underestimation of the true burden of NCDs and the corresponding inadequacies in health service provision. As NCDs constitute a growing proportion of the disease burden in South Africa, the lack of comprehensive data further complicates efforts to accurately gauge progress towards UHC and to identify areas most in need of intervention. The current UHC index score of 51.6, therefore, not only reflects existing service coverage gaps but also highlights the critical need for improved data collection and analysis to better inform health policy and resource allocation, particularly in relation to NCDs. Without addressing these data challenges, South Africa may struggle to fully understand and address the barriers to achieving SDG 3.8 and improving overall population health outcomes.104
Health services indicators by province are presented in Table 11.
Table 11.Health services indicators by province
| Indicator |
Period |
Sex|Age|Series|Cat |
SA |
EC |
FS |
GP |
KZ |
LP |
MP |
NC |
NW |
WC |
Ref |
| Average length of stay - total |
2022/23 |
DHIS |
6,2 |
6,9 |
5,7 |
7,2 |
6,4 |
5,4 |
4,7 |
5,3 |
6,1 |
5,6 |
a |
| Average length of stay (district hospitals) |
2022/23 |
DHIS |
4,3 |
4,7 |
3,0 |
4,7 |
5,0 |
4,2 |
4,3 |
3,1 |
4,3 |
3,6 |
a |
| Birth registration coverage |
2020 |
both sexes Live biths of current registration |
70,8 |
|
|
|
|
|
|
|
|
|
b |
| 2021 |
both sexes Live biths of current registration |
74,6 |
|
|
|
|
|
|
|
|
|
b |
| 2022 |
both sexes Live biths of current registration |
78,0 |
|
|
|
|
|
|
|
|
|
b |
| Complaints resolution rate |
2022/23 |
DHIS |
90,5 |
89,3 |
80,8 |
90,8 |
93,0 |
91,1 |
87,1 |
|
93,4 |
|
a |
| Complaints resolution rate within 25 working days |
2022/23 |
DHIS |
95,4 |
95,6 |
90,7 |
95,9 |
94,7 |
97,2 |
96,0 |
|
97,5 |
|
a |
| Death under 5 years against live birth rate |
2022/23 |
both sexes DHIS |
1,8 |
2,1 |
2,4 |
1,9 |
1,8 |
1,9 |
1,8 |
2,2 |
1,9 |
1,3 |
a |
| Hospital beds per 10 000 target population |
Mar 2023 |
DHIS 2000-2030 District Hospital |
5,8 |
10,1 |
6,4 |
2,1 |
7,8 |
7,4 |
7,0 |
5,1 |
3,4 |
5,2 |
a |
| DHIS 2000-2030 public sector |
20,3 |
22,0 |
25,9 |
14,4 |
20,0 |
13,7 |
11,2 |
16,6 |
11,8 |
18,3 |
a |
| Inpatient bed utilisation rate - total |
2022/23 |
DHIS |
66,9 |
56,5 |
67,7 |
77,2 |
59,3 |
68,5 |
64,4 |
31,1 |
73,2 |
84,9 |
a |
| Inpatient bed utilisation rate (district hospitals) |
2022/23 |
DHIS |
60,0 |
46,2 |
52,1 |
67,7 |
53,7 |
66,6 |
61,7 |
47,4 |
62,7 |
92,8 |
a |
| Inpatient crude death rate |
2022/23 |
both sexes DHIS |
4,6 |
6,2 |
4,2 |
5,3 |
4,5 |
4,6 |
4,4 |
4,8 |
4,8 |
3,2 |
a |
| Inpatient deaths - total |
2022/23 |
both sexes DHIS |
165 824 |
24 975 |
12 046 |
37 717 |
31 654 |
16 701 |
10 695 |
3 436 |
9 247 |
19 353 |
a |
| International Health Regulations (IHR) core capacity index |
2022 |
WHO |
73,0 |
|
|
|
|
|
|
|
|
|
c |
| Number of beds |
Mar 2023 |
DHIS central hospital |
10 496 |
576 |
618 |
6 063 |
846 |
|
|
|
|
2 393 |
a |
| DHIS district hospital |
30 749 |
6 128 |
1 610 |
2 688 |
8 213 |
4 233 |
2 973 |
569 |
1 268 |
3 067 |
a |
| DHIS provincial hospital |
10 493 |
1 782 |
588 |
2 410 |
1 783 |
1 042 |
725 |
635 |
1 236 |
292 |
a |
| DHIS public sector |
88 785 |
13 284 |
6 571 |
18 214 |
21 000 |
7 856 |
4 767 |
1 865 |
4 465 |
10 763 |
a |
| DHIS regional hospital |
20 276 |
2 082 |
1 113 |
5 106 |
7 013 |
1 561 |
877 |
227 |
847 |
1 450 |
a |
| DHIS specialised psychiatric hospital |
9 924 |
1 286 |
760 |
1 446 |
2 452 |
931 |
|
131 |
1 114 |
1 804 |
a |
| DHIS specialised TB hospital |
2 597 |
1 143 |
|
|
203 |
89 |
192 |
44 |
|
926 |
a |
| Number of health facilities |
Mar 2023 |
DHIS district hospital |
250 |
65 |
25 |
12 |
39 |
30 |
23 |
11 |
12 |
33 |
a |
| DHIS fixed chc/cdc |
352 |
41 |
10 |
40 |
23 |
26 |
57 |
33 |
48 |
74 |
a |
| DHIS fixed clinic |
3 151 |
735 |
211 |
333 |
596 |
455 |
241 |
129 |
266 |
185 |
a |
| DHIS military hospital |
3 |
|
1 |
1 |
|
|
|
|
|
1 |
a |
| DHIS national central hospital |
9 |
1 |
1 |
4 |
1 |
|
|
|
|
2 |
a |
| DHIS private hospital |
470 |
27 |
30 |
181 |
102 |
17 |
22 |
11 |
21 |
59 |
a |
| DHIS provincial tertiary hospital |
18 |
3 |
1 |
3 |
3 |
2 |
2 |
1 |
2 |
1 |
a |
| DHIS regional hospital |
48 |
5 |
4 |
9 |
13 |
5 |
3 |
1 |
3 |
5 |
a |
| DHIS specialised hospital |
8 |
2 |
|
3 |
3 |
|
|
|
|
|
a |
| DHIS specialised psychiatric hospital |
24 |
4 |
1 |
3 |
6 |
3 |
|
1 |
2 |
4 |
a |
| DHIS specialised TB hospital |
27 |
10 |
|
|
4 |
1 |
5 |
1 |
|
6 |
a |
| OHH headcount under 5 years coverage |
2022/23 |
DHIS |
119,3 |
67,6 |
101,2 |
91,3 |
169,1 |
141,9 |
108,4 |
91,1 |
100,7 |
146,1 |
a |
| OPD new client not referred rate |
2022/23 |
DHIS |
42,6 |
44,8 |
45,5 |
27,6 |
46,8 |
62,8 |
52,6 |
66,5 |
46,6 |
11,3 |
a |
| OPD new client not referred rate (district hospitals) |
2022/23 |
DHIS |
58,3 |
60,2 |
56,0 |
64,9 |
54,7 |
71,7 |
63,5 |
69,6 |
52,2 |
14,8 |
a |
| Patient Day Equivalent |
2022/23 |
DHIS |
30 414 491 |
3 696 383 |
2 011 660 |
7 283 110 |
6 388 188 |
2 808 595 |
1 789 898 |
572 098 |
1 629 276 |
4 235 283 |
a |
| DHIS district hospital |
7 727 019 |
1 124 148 |
378 799 |
793 972 |
1 802 419 |
1 192 190 |
852 265 |
142 499 |
319 434 |
1 121 293 |
a |
| PHC doctor clinical work load |
2022/23 |
DHIS |
16,7 |
15,6 |
18,0 |
12,9 |
19,4 |
23,4 |
11,9 |
12,8 |
12,1 |
22,3 |
a |
| PHC heacount total |
2022/23 |
both sexes all ages DHIS |
106 401 284 |
14 117 664 |
106 401 284 |
19 724 563 |
24 714 031 |
13 046 940 |
8 133 735 |
2 537 807 |
7 003 680 |
12 063 928 |
a |
| PHC headcount 5 years and older |
2022/23 |
both sexes DHIS |
88 349 611 |
11 916 087 |
4 284 857 |
16 370 117 |
20 626 617 |
10 414 507 |
6 603 275 |
2 164 037 |
5 828 198 |
10 141 916 |
a |
| PHC headcount under 5 years |
2022/23 |
DHIS |
18 051 673 |
2 201 577 |
774 079 |
3 354 446 |
4 087 414 |
2 632 433 |
1 530 460 |
373 770 |
1 175 482 |
1 922 012 |
a |
| PHC professional nurse clinical work load |
2022/23 |
DHIS |
23,0 |
25,8 |
24,5 |
21,9 |
27,3 |
20,5 |
25,9 |
17,0 |
17,0 |
20,5 |
a |
| PHC utilisation rate |
2022/23 |
DHIS |
1,7 |
2,1 |
1,7 |
1,2 |
2,1 |
2,1 |
1,7 |
1,9 |
1,7 |
1,7 |
a |
| PHC utilisation rate under 5 years |
2022/23 |
DHIS |
3,2 |
3,3 |
3,0 |
2,6 |
3,3 |
4,1 |
3,2 |
3,0 |
2,9 |
3,4 |
a |
| Universal health coverage: service coverage index |
2021 |
WHO |
71,0 |
|
|
|
|
|
|
|
|
|
c |
|
2023 |
GBD 2016 scaled |
51,6 |
|
|
|
|
|
|
|
|
|
d |
Reference notes
a webDHIS.16
b Stats SA Live Births 2022.42
c World Health Statistics, 2023.24
d GBD 2016 SDGs.105
Definitions
• Inpatient deaths - total [Number]: An inpatient death is a death recorded against an admitted inpatient, including the death of a patient admitted earlier on the same day. The total is specialities plus all others that do not appear on the identified specialities.
• Number of beds [Number]: Total number of beds in health facility.
• Number of health facilities [Number].
• Patient Day Equivalent [Number]: The sum of Inpatient days total x 1, Day patient total x 0.5, and OPD/Emergency total headcount x 0.3333333.
• PHC headcount total [Number].
• PHC headcount 5 years and older [Number].
• PHC headcount under 5 years [Number]: All individual clients not yet reached five years (60 months) seen for Primary Health Care services at a facility.
• Average length of stay - total [Days]: The average number of patients days that an admitted patients spends in hospital before separation.
• Average length of stay (district hospitals) [Days]: The average number of patient days that an admitted patient spends in hospital before separation.
• Birth registration coverage [Percentage]: Percentage of births that are registered within one month of age in a civil registration system.
• Complaints resolution rate [Percentage]: Complaints resolved as a proportion of complaints received.
• Complaints resolution rate within 25 working days [Percentage]: Complaints resolved within 25 working days as a proportion of all complaints resolved.
• Death registration coverage [Percentage]: Percentage of deaths that are registered (with age and sex).
• Death under 5 years against live birth rate [Percentage]: Children under 5 years who died during their stay in the facility as a proportion of all live births.
• Hospital beds per 10 000 target population [per 10 000 uninsured]: Number of inpatient beds per 10 000 target population. For public sector beds, the uninsured population is used as the target.
• Inpatient bed utilisation rate - total [Percentage]: A measure of the average number of beds that are occupied - expressed as the proportion of all available bed days, which is calculated as the number of actual beds multiplied by the average number of days in a month (30.42).
• Inpatient bed utilisation rate (district hospitals) [Percentage]: A measure of the average number of beds that are occupied - expressed as the proportion of all available bed days, which is calculated as the number of actual beds multiplied by the average number of days in a month (30.42).
• Inpatient crude death rate [Percentage]: Proportion of admitted clients/separations who died during hospital stay. Inpatient separations is the total of day clients, inpatient discharges, inpatient deaths and inpatient transfer outs.
• International Health Regulations (IHR) core capacity index [Percentage]: Percentage of attributes of 13 core capacities that have been attained at a specific point in time. The 13 core capacities are: (1) National legislation, policy and financing; (2) Coordination and National Focal Point communications; (3) Surveillance; (4) Response; (5) Preparedness; (6) Risk communication; (7) Human resources; (8) Laboratory; (9) Points of entry; (10) Zoonotic events; (11) Food safety; (12) Chemical events; (13) Radionuclear emergencies.
• OHH headcount under 5 years coverage [Percentage]: Children under 5 years in population who received care during Ward- Based Outreach Team visits as a proportion of population under 5 years.
• OPD new client not referred rate (district hospitals) [Percentage]: OPD clinic new cases (seeking medical attention for a condition for the first time) that report to the OPD department without being referred from a PHC facility or doctor (including General Practitioners) during the reporting period as a proportion of OPD new clients.
• OPD new client not referred rate [Percentage]: New OPD clients not referred as a proportion of OPD new clients - total.
• PHC doctor clinical work load [Clients per doctor per day]: Average number of clients seen per doctor per clinical work day. This includes doctors employed in the public and private sector.
• PHC professional nurse clinical work load [Clients per nurse per day]: Average number of clients seen per professional nurse per professional nurse clinical work day.
• PHC utilisation rate [Average number of visits per person]: Average number of PHC visits per person per year in the population.
• PHC utilisation rate under 5 years [Average number of visits per person under 5 years].
• Average number of PHC visits per year per person under 5 years of age in the population.
• Universal health coverage: service coverage index [Scale 0-100]: Coverage of essential health services (defined as the average coverage of essential services based on tracer interventions that include reproductive, maternal, newborn and child health, infectious diseases, non-communicable diseases and service capacity and access, among the general and the most disadvantaged population). Calculated as the geometric mean of the index score for each of the 4 categories of the index.
Health personnel
It is important to note that the health personnel data reported in Table 12 and Table 13 only reflect the position in the public sector, with the uninsured population used as the denominator. Reconciling PERSAL data with the total number of health professionals registered with the respective statutory health councils is also fraught with difficulty, as those sources cannot show how many registered persons are non-practising or have emigrated. The National Department of Health Strategic Plan 2020/21-2024/25 includes a commitment to “improve equity, training and enhance management of Human Resources for Health”, in order to improve the provision of care (Goal 3).106(p77) However, evidence to show that the Human Resources for Health Operational Plan has, in fact, been ‘augmented’, is lacking.
Challenges in human resources for health
Despite commitments to fill critical vacant posts, integrate community health workers into the public health system, consolidate nursing colleges, and supplement the production of medical practitioners and other health professionals, there has been persistent media coverage of regression, of frozen posts, and unemployed graduates. The inability to employ newly graduated health professionals has several long-term implications. First, it contributes to an underutilisation of skilled labour, leading to a mismatch between the availability of trained professionals and the needs of the health system. This mismatch can result in increased workloads for existing staff, higher burnout rates and, ultimately, a decline in the quality of care provided to patients. As identified in the 2030 Human Resources for Health Strategy: Investing in the Health Workforce for Universal Health Coverage, “Even when a projected need has been determined, the mechanisms and fiscal arrangements required to support the implementation of the HRH plans have been ineffective.”107(p46)
Monitoring and evaluation
Of specific relevance to this paper, the Strategy also stated: “Insufficient information hampers the monitoring and evaluation of HRH plans, contributing to the lack of or inadequate implementation” and “Access to private sector data is limited and thus poorly integrated into the national picture.”107(p50)
Table 12.Number of health personnel practising in the public sector by province
| Indicator |
Period |
Sex|Age|Series|Cat |
SA |
EC |
FS |
GP |
KZ |
LP |
MP |
NC |
NW |
WC |
Ref |
| Number of clinical associates registered |
2022 |
both sexes all ages HPCSA |
1 038 |
|
|
|
|
|
|
|
|
|
a |
| Number of CS clinical psychologists |
2023 Mar |
both sexes public sector |
76 |
1 |
2 |
43 |
8 |
5 |
3 |
2 |
6 |
6 |
b |
| Number of CS dentists |
2023 Mar |
both sexes public sector |
166 |
16 |
25 |
26 |
42 |
6 |
13 |
12 |
10 |
16 |
b |
| Number of CS dieticians |
2023 Mar |
both sexes public sector |
222 |
16 |
21 |
52 |
51 |
19 |
18 |
13 |
25 |
7 |
b |
| Number of CS doctors |
2023 Mar |
both sexes public sector |
2 264 |
324 |
119 |
315 |
278 |
300 |
312 |
68 |
263 |
285 |
b |
| Number of CS environmental health practitioners |
2023 Mar |
both sexes public sector |
170 |
2 |
13 |
34 |
7 |
41 |
23 |
14 |
36 |
|
b |
| Number of CS nurses |
2023 Mar |
both sexes public sector |
2 982 |
636 |
181 |
811 |
373 |
201 |
248 |
28 |
199 |
305 |
b |
| Number of CS occupational therapists |
2023 Mar |
both sexes public sector |
355 |
49 |
25 |
81 |
83 |
14 |
29 |
22 |
39 |
13 |
b |
| Number of CS pharmacists |
2023 Mar |
both sexes public sector |
599 |
61 |
36 |
90 |
137 |
56 |
54 |
37 |
76 |
52 |
b |
| Number of CS physiotherapists |
2023 Mar |
both sexes public sector |
419 |
61 |
32 |
98 |
76 |
21 |
34 |
28 |
43 |
26 |
b |
| Number of CS radiographers |
2023 Mar |
both sexes public sector |
332 |
30 |
13 |
81 |
71 |
18 |
30 |
15 |
39 |
35 |
b |
| Number of CS speech therapists |
2023 Mar |
both sexes public sector |
244 |
17 |
11 |
66 |
73 |
9 |
26 |
13 |
23 |
6 |
b |
| Number of dental practitioners |
2023 Mar |
both sexes public sector |
984 |
152 |
41 |
238 |
108 |
152 |
78 |
26 |
55 |
134 |
b |
| Number of dental specialists |
2023 Mar |
both sexes public sector |
129 |
|
1 |
91 |
2 |
4 |
1 |
|
|
30 |
b |
| Number of dental therapists |
2023 Mar |
both sexes public sector |
349 |
19 |
1 |
43 |
93 |
126 |
30 |
23 |
12 |
2 |
b |
| Number of enrolled nurses |
2023 Mar |
both sexes public sector |
29 806 |
3 560 |
1 131 |
7 159 |
9 611 |
2 928 |
1 182 |
238 |
1 076 |
2 921 |
b |
| Number of environmental health practitioners |
2023 Mar |
both sexes public sector |
441 |
18 |
88 |
135 |
75 |
26 |
47 |
18 |
33 |
1 |
b |
| Number of medical practitioners |
2023 Mar |
both sexes public sector |
17 486 |
2 093 |
775 |
4 538 |
3 915 |
1 483 |
1 025 |
382 |
1 063 |
2 212 |
b |
| Number of medical researchers |
2023 Mar |
both sexes public sector |
122 |
4 |
|
17 |
81 |
10 |
1 |
1 |
|
8 |
b |
| Number of medical specialists |
2023 Mar |
both sexes public sector |
4 759 |
218 |
378 |
1 855 |
806 |
74 |
64 |
37 |
155 |
1 172 |
b |
| Number of nursing assistants |
2023 Mar |
both sexes public sector |
34 393 |
5 305 |
2 210 |
6 860 |
5 422 |
4 454 |
2 119 |
841 |
2 886 |
4 296 |
b |
| Number of occupational therapists |
2023 Mar |
both sexes public sector |
1 071 |
107 |
48 |
282 |
145 |
195 |
62 |
27 |
45 |
160 |
b |
| Number of optometrists and opticians |
2023 Mar |
both sexes public sector |
253 |
6 |
8 |
53 |
65 |
106 |
7 |
2 |
4 |
2 |
b |
| Number of pharmacists |
2023 Mar |
both sexes public sector |
5 958 |
930 |
404 |
1 240 |
865 |
730 |
375 |
111 |
261 |
1 042 |
b |
| Number of physiotherapists |
2023 Mar |
both sexes public sector |
1 172 |
138 |
49 |
223 |
261 |
165 |
76 |
30 |
72 |
158 |
b |
| Number of professional nurses |
2023 Mar |
both sexes public sector |
75 358 |
11 293 |
2 557 |
15 720 |
18 294 |
8 603 |
6 587 |
1 497 |
5 253 |
5 554 |
b |
| Number of psychologists |
2023 Mar |
both sexes public sector |
777 |
73 |
29 |
232 |
103 |
124 |
55 |
14 |
43 |
104 |
b |
| Number of radiographers |
2023 Mar |
both sexes public sector |
2 970 |
380 |
150 |
888 |
587 |
214 |
122 |
66 |
116 |
447 |
b |
| Number of speech therapists and audiologists |
2023 Mar |
both sexes public sector |
588 |
57 |
8 |
151 |
148 |
63 |
42 |
13 |
30 |
76 |
b |
| Number of student nurses |
2023 Mar |
both sexes public sector |
824 |
|
|
72 |
517 |
6 |
228 |
|
1 |
|
b |
Reference notes
a HPCSA, 2023.108
b PERSAL.46
Table 13.Health personnel per 100 000 uninsured population by province
| Indicator |
Period |
Sex|Age|Series|Cat |
SA |
EC |
FS |
GP |
KZ |
LP |
MP |
NC |
NW |
WC |
Ref |
| Density of dentistry personnel (per 10 000 population) |
2013-2021 |
both sexes WHO |
1,1 |
|
|
|
|
|
|
|
|
|
a |
| Density of midwifery personnel (per 10 000 population) |
2013-2021 |
both sexes WHO |
50,1 |
|
|
|
|
|
|
|
|
|
a |
| Density of pharmaceutical personnel (per 10 000 population) |
2013-2021 |
both sexes WHO |
2,7 |
|
|
|
|
|
|
|
|
|
a |
| Density of physicans (per 10 000 population) |
2013-2021 |
both sexes WHO |
8,1 |
|
|
|
|
|
|
|
|
|
a |
| Dental practitioners per 100 000 population |
2023 Mar |
both sexes public sector |
2,2 |
2,8 |
2,6 |
2,1 |
1,4 |
2,8 |
2,1 |
3,4 |
1,7 |
2,5 |
b |
| Dental specialists per 100 000 population |
2023 Mar |
both sexes public sector |
0,3 |
|
0,0 |
0,7 |
0,0 |
0,1 |
0,0 |
|
|
0,5 |
b |
| Dental therapists per 100 000 population |
2023 Mar |
both sexes public sector |
0,7 |
0,3 |
0,0 |
0,3 |
0,9 |
2,2 |
0,7 |
2,0 |
0,3 |
0,0 |
b |
| Enrolled nurses per 100 000 population |
2023 Mar |
both sexes public sector |
56,6 |
58,8 |
44,6 |
56,8 |
91,7 |
51,2 |
27,7 |
21,2 |
28,4 |
49,6 |
b |
| Environmental health practitioners per 100 000 population |
2023 Mar |
both sexes public sector |
1,2 |
0,3 |
4,0 |
1,3 |
0,8 |
1,2 |
1,6 |
2,8 |
1,8 |
0,0 |
b |
| Medical practitioners per 100 000 population |
2023 Mar |
both sexes public sector |
37,5 |
39,9 |
35,3 |
38,5 |
40,0 |
31,2 |
31,3 |
40,0 |
35,1 |
42,4 |
b |
| Medical researchers per 100 000 population |
2023 Mar |
both sexes public sector |
0,2 |
0,1 |
|
0,1 |
0,8 |
0,2 |
0,0 |
0,1 |
|
0,1 |
b |
| Medical specialists per 100 000 population |
2023 Mar |
both sexes public sector |
9,0 |
3,6 |
14,9 |
14,7 |
7,7 |
1,3 |
1,5 |
3,3 |
4,1 |
19,9 |
b |
| Nursing assistants per 100 000 population |
2023 Mar |
both sexes public sector |
65,4 |
87,7 |
87,2 |
54,4 |
51,7 |
77,8 |
49,6 |
74,8 |
76,3 |
73,0 |
b |
| Occupational therapists per 100 000 population |
2023 Mar |
both sexes public sector |
2,7 |
2,6 |
2,9 |
2,9 |
2,2 |
3,7 |
2,1 |
4,4 |
2,2 |
2,9 |
b |
| Optometrists per 100 000 population |
2023 Mar |
both sexes public sector |
0,5 |
0,1 |
0,3 |
0,4 |
0,6 |
1,9 |
0,2 |
0,2 |
0,1 |
0,0 |
b |
| Pharmacists per 100 000 population |
2023 Mar |
both sexes public sector |
12,5 |
16,4 |
17,4 |
10,5 |
9,6 |
13,7 |
10,0 |
13,2 |
8,9 |
18,6 |
b |
| Physiotherapists per 100 000 population |
2023 Mar |
both sexes public sector |
3,0 |
3,3 |
3,2 |
2,5 |
3,2 |
3,3 |
2,6 |
5,2 |
3,0 |
3,1 |
b |
| Professional nurses per 100 000 population |
2023 Mar |
both sexes public sector |
148,9 |
197,1 |
108,0 |
131,1 |
178,1 |
153,9 |
160,1 |
135,6 |
144,2 |
99,5 |
b |
| Psychologists per 100 000 population |
2023 Mar |
both sexes public sector |
1,6 |
1,2 |
1,2 |
2,2 |
1,1 |
2,3 |
1,4 |
1,4 |
1,3 |
1,9 |
b |
| Radiographers per 100 000 population |
2023 Mar |
both sexes public sector |
6,3 |
6,8 |
6,4 |
7,7 |
6,3 |
4,1 |
3,6 |
7,2 |
4,1 |
8,2 |
b |
| Speech therapists and audiologists per 100 000 population |
2023 Mar |
both sexes public sector |
1,6 |
1,2 |
0,8 |
1,7 |
2,1 |
1,3 |
1,6 |
2,3 |
1,4 |
1,4 |
b |
| Student nurses per 100 000 population |
2023 Mar |
both sexes public sector |
1,6 |
|
|
0,6 |
4,9 |
0,1 |
5,3 |
|
0,0 |
|
b |
Reference notes
a World Health Statistics, 2023.24
b PERSAL.46
Definitions
• Indicators are calculated as the number of the specified cadre of health professional per 100 000 uninsured population, as calculated using the webDHIS 2000-30 population time series and the Insight Actuaries modelled estimates for medical schemes coverage at district level circa 2018.
Health financing
Tables 14 to 16 provide the basic financial indicators for the public health sector over time. Between 2012/13 and 2022/23, there has been almost a doubling in total expenditure in terms of provincial and local government expenditure on health, from R125.5 billion to R247.7 billion per annum (Table 14). Whether this has been accompanied by a commensurate improvement in health outcomes is questionable, as has been shown in the preceding sections of this paper.
Primary health care expenditure
The shift towards primary health care is evident in the proportion of expenditure on district health systems, which represented 47.0% of provincial and local government health expenditure at a national level in 2022/23 (Table 15). That this proportion varied widely among provinces, from 31.8% in Gauteng to 65.5% in Limpopo, is reflective of the relative contribution of higher level hospital services among provinces. The relative changes between financial years 2021/22 and 2022/23 per province are also depicted in Figure 24.
Health services in the public sector are still almost exclusively dependent on the fiscus. As shown in Table 16, the proportion of provincial and local government health expenditure that is provided by development partners (external donors) remains modest, at US$1.40 per capita in 2021 (including support for medical research).
Medical scheme coverage
Medical scheme coverage, as estimated from both the Stats SA General Household Survey34 and the annual reports of the Council for Medical Schemes,48 remains around the 15% mark. However, according to the 2022 report from the Council for Medical Schemes, total disbursements in the insured sector in 2022 were R224.1 billion.48 This represented a 9.2% increase from the amount reported for 2021 of R205.3 billion. The amount spent in the insured private sector was thus comparable to the total spent in the public health sector in 2022. Consolidation of the number of medical schemes continues, with the total number declining from 144 in 2000 to 72 in 2022. Modest increases in the number of beneficiaries covered by both open (30 930) and restricted schemes (69 457) were recorded between 2021 and 2022, bringing the total number of insured persons to 9.04 million. Notably, in 2022, ten government-linked or funded medical schemes represented 72% of all restricted scheme beneficiaries and 33% of the total number of beneficiaries.
Table 14.Trends in overall provincial and local government health expenditure by programme (Rand million, nominal prices), 2012/13 – 2022/23
| Rand million |
Financial Year |
| Programme |
FY 2013 |
FY 2014 |
FY 2015 |
FY 2016 |
FY 2017 |
FY 2018 |
FY 2019 |
FY 2020 |
FY 2021 |
FY 2022 |
FY 2023 |
| 1. Administration |
3,019 |
3,578 |
3,599 |
4,313 |
4,462 |
4,690 |
5,129 |
5,368 |
8,799 |
7,596 |
7,273 |
| 2. District Health Services |
53,586 |
57,991 |
64,181 |
69,854 |
76,540 |
83,671 |
90,978 |
98,688 |
109,448 |
115,084 |
116,406 |
| 3. Emergency Health Services |
5,079 |
5,352 |
5,556 |
6,025 |
6,435 |
7,380 |
7,671 |
8,394 |
8,660 |
8,791 |
9,817 |
| 4. Provincial Hospital Services |
27,741 |
26,420 |
28,694 |
29,576 |
29,675 |
32,262 |
34,275 |
36,609 |
37,623 |
39,134 |
40,607 |
| 5. Central Hospital Services |
18,822 |
23,559 |
25,804 |
29,529 |
33,736 |
37,437 |
41,120 |
44,608 |
47,516 |
47,227 |
50,010 |
| 6. Health Sciences and Training |
3,755 |
4,039 |
4,248 |
4,529 |
5,107 |
4,916 |
5,037 |
5,115 |
4,796 |
4,792 |
5,270 |
| 7. Health Care Support Services |
1,640 |
1,877 |
1,322 |
2,834 |
1,796 |
1,806 |
4,661 |
2,301 |
3,469 |
3,073 |
2,936 |
| 8. Health Facilities Management |
8,967 |
7,895 |
7,491 |
8,514 |
8,316 |
8,651 |
9,014 |
9,844 |
11,526 |
10,433 |
10,236 |
| Local government expenditure |
2,859 |
2,869 |
3,389 |
3,730 |
4,103 |
4,199 |
4,858 |
4,828 |
5,392 |
5,158 |
5,140 |
| Other |
4 |
|
|
|
|
- |
- |
|
- |
-14M |
- |
| Grand Total |
125,473 |
133,581 |
144,283 |
158,903 |
170,171 |
185,013 |
202,744 |
215,755 |
237,229 |
241,273 |
247,697 |
Note: ‘Other’ includes any other expenditure not indicated as being allocated to any of the above budget programmes.
Source: National Treasury database.45
Table 15.Provincial and local government health expenditure per province by programme (Rand million), 2022/23
| Rand million |
Financial Year 2022/23 |
| Programme |
SA |
EC |
FS |
GP |
KZ |
LP |
MP |
NC |
NW |
WC |
| 1. Administration |
7 273 |
847 |
324 |
1 826 |
1 120 |
280 |
333 |
282 |
1 204 |
1 057 |
| 2. District Health Services |
116 406 |
15 077 |
6 005 |
19 494 |
27 224 |
15 406 |
10 497 |
2 785 |
7 866 |
12 050 |
| 3. Emergency Health Services |
9 817 |
1 453 |
1 004 |
2 011 |
1 668 |
1 039 |
439 |
419 |
481 |
1 303 |
| 4. Provincial Hospital Services |
40 607 |
3 927 |
1 688 |
11 082 |
12 379 |
2 718 |
1 680 |
454 |
2 174 |
4 507 |
| 5. Central Hospital Services |
50 010 |
4 714 |
2 893 |
21 485 |
5 663 |
2 091 |
1 727 |
1 259 |
2 250 |
7 928 |
| 6. Health Sciences and Training |
5 270 |
986 |
324 |
638 |
1 339 |
639 |
519 |
172 |
269 |
384 |
| 7. Health Care Support Services |
2 936 |
115 |
159 |
437 |
222 |
225 |
282 |
133 |
776 |
585 |
| 8. Health Facilities Management |
10 236 |
1 072 |
791 |
1 665 |
1 913 |
1 016 |
1 532 |
407 |
725 |
1 115 |
| Local government expenditure |
5 140 |
261 |
48 |
2 641 |
620 |
100 |
115 |
33 |
81 |
1 243 |
|
Grand Total
|
247 697 |
28 450 |
13 237 |
61 281 |
52 148 |
23 514 |
17 124 |
5 945 |
15 828 |
30 172 |
Source: National Treasury database.45

Figure 24.Percentage of expenditure per programme by province, 2021/22 compared to 2022/23
Source: National Treasury database.45
Table 16.Health financing indicators by province
| Indicator |
Period |
Sex|Age|Series|Cat |
SA |
EC |
FS |
GP |
KZ |
LP |
MP |
NC |
NW |
WC |
Ref |
| Claims ratio |
2020 |
both sexes all ages med schemes |
81,4 |
|
|
|
|
|
|
|
|
|
a |
| 2021 |
both sexes all ages med schemes |
90,9 |
|
|
|
|
|
|
|
|
|
b |
| 2022 |
both sexes all ages med schemes |
94,0 |
|
|
|
|
|
|
|
|
|
c |
| Expenditure per patient day equivalent (district hospitals) |
2020/21 |
BAS real 2022/23 prices |
4 543 |
4 962 |
3 950 |
5 402 |
4 687 |
4 505 |
4 062 |
4 716 |
4 890 |
3 785 |
d |
| 2021/22 |
BAS real 2022/23 prices |
3 920 |
3 102 |
3 628 |
4 828 |
4 435 |
4 232 |
3 778 |
4 268 |
4 363 |
3 277 |
d |
| 2022/23 |
BAS real 2022/23 prices |
3 783 |
3 819 |
3 285 |
4 230 |
3 942 |
4 030 |
3 588 |
3 620 |
4 425 |
3 077 |
d |
| Medical scheme beneficiaries |
2020 |
both sexes all ages med schemes |
8 886 933 |
664 093 |
396 451 |
3 435 040 |
1 289 664 |
472 055 |
551 551 |
181 609 |
456 057 |
1 386 299 |
a |
| 8 895 152 |
664 509 |
396 758 |
3 436 286 |
1 290 329 |
456 321 |
555 404 |
181 845 |
472 351 |
1 387 206 |
b |
| 2021 |
both sexes all ages med schemes |
8 938 872 |
660 064 |
400 721 |
3 496 871 |
1 274 134 |
468 362 |
556 393 |
193 501 |
469 846 |
1 384 260 |
b |
| 2022 |
both sexes all ages med schemes |
9 037 439 |
659 733 |
408 492 |
3 524 601 |
1 284 220 |
485 310 |
566 647 |
187 979 |
489 829 |
1 399 899 |
c |
| female med schemes |
4 847 929 |
|
|
|
|
|
|
|
|
|
c |
| male med schemes |
4 189 510 |
|
|
|
|
|
|
|
|
|
c |
| Medical scheme coverage |
2020 |
both sexes all ages med schemes |
14,8 |
7,0 |
4,0 |
39,0 |
15,0 |
5,0 |
6,0 |
2,0 |
5,0 |
16,0 |
a |
| 2021 |
both sexes all ages GHS |
16,1 |
10,6 |
16,3 |
24,0 |
10,5 |
8,2 |
9,1 |
19,6 |
15,3 |
23,7 |
e |
| both sexes all ages med schemes |
14,9 |
7,0 |
4,0 |
39,0 |
14,0 |
5,0 |
6,0 |
2,0 |
5,0 |
15,0 |
b |
| 2022 |
both sexes all ages GHS |
15,8 |
10,6 |
14,5 |
22,2 |
11,1 |
8,9 |
10,2 |
15,7 |
13,6 |
25,2 |
f |
| both sexes all ages med schemes |
14,9 |
7,3 |
4,5 |
39,0 |
14,2 |
5,4 |
6,3 |
2,1 |
5,4 |
15,5 |
c |
| female all ages med schemes |
53,6 |
|
|
|
|
|
|
|
|
|
c |
| male all ages med schemes |
46,4 |
|
|
|
|
|
|
|
|
|
c |
| Pensioner ratio |
2020 |
both sexes all ages med schemes |
8,9 |
|
|
|
|
|
|
|
|
|
a |
| 2021 |
both sexes med schemes |
9,0 |
|
|
|
|
|
|
|
|
|
b |
| female med schemes |
10,0 |
|
|
|
|
|
|
|
|
|
b |
| male med schemes |
7,8 |
|
|
|
|
|
|
|
|
|
b |
| 2022 |
both sexes med schemes |
9,3 |
|
|
|
|
|
|
|
|
|
c |
| female med schemes |
10,3 |
|
|
|
|
|
|
|
|
|
c |
| male med schemes |
8,1 |
|
|
|
|
|
|
|
|
|
c |
| Proportion of population with large household expenditures on health as a share of total household expenditure or income |
2010-2018 |
both sexes WHO >10% |
1,4 |
|
|
|
|
|
|
|
|
|
g |
| both sexes WHO >25% |
0,1 |
|
|
|
|
|
|
|
|
|
g |
| 2012-2020 |
both sexes WHO >10% |
1,0 |
|
|
|
|
|
|
|
|
|
h |
| both sexes WHO >25% |
0,1 |
|
|
|
|
|
|
|
|
|
h |
| 2013-2021 |
both sexes WHO >10% |
1,0 |
|
|
|
|
|
|
|
|
|
i |
| both sexes WHO >25% |
0,1 |
|
|
|
|
|
|
|
|
|
i |
| Provincial & LG District Health Services expenditure per capita (uninsured) |
2020/21 |
BAS real 2022/23 prices |
2 519 |
2 861 |
2 577 |
2 005 |
2 785 |
2 875 |
2 547 |
2 676 |
2 246 |
2 495 |
d |
| 2021/22 |
BAS real 2022/23 prices |
2 496 |
2 680 |
2 487 |
1 930 |
2 880 |
2 755 |
2 688 |
2 775 |
2 395 |
2 424 |
d |
| 2022/23 |
BAS real 2022/23 prices |
2 332 |
2 509 |
2 387 |
1 771 |
2 662 |
2 726 |
2 521 |
2 531 |
2 123 |
2 301 |
d |
| Provincial & LG PHC expenditure per capita (uninsured) |
2020/21 |
BAS real 2022/23 prices |
1 591 |
1 539 |
1 793 |
1 552 |
1 886 |
1 349 |
1 416 |
1 658 |
1 383 |
1 595 |
d |
| 2021/22 |
BAS real 2022/23 prices |
1 569 |
1 480 |
1 718 |
1 436 |
1 996 |
1 328 |
1 446 |
1 715 |
1 412 |
1 511 |
d |
| 2022/23 |
BAS real 2022/23 prices |
1 479 |
1 397 |
1 644 |
1 339 |
1 818 |
1 367 |
1 355 |
1 590 |
1 378 |
1 428 |
d |
| Provincial & LG PHC expenditure per PHC headcount |
2020/21 |
BAS real 2022/23 prices |
842,1 |
720,5 |
931,7 |
1 078,0 |
838,8 |
610,7 |
791,6 |
815,7 |
793,3 |
928,1 |
d |
| 2021/22 |
BAS real 2022/23 prices |
790,9 |
655,3 |
902,8 |
927,9 |
855,9 |
588,2 |
776,0 |
809,8 |
783,9 |
783,6 |
d |
| 2022/23 |
BAS real 2022/23 prices |
719,4 |
599,7 |
817,9 |
836,7 |
761,5 |
595,9 |
701,3 |
697,5 |
732,2 |
683,6 |
d |
| Total net official development assistance to medical research and basic health sectors per capita (US$), by recipient country |
2019 |
WHO |
1,9 |
|
|
|
|
|
|
|
|
|
g |
| 2020 |
WHO |
0,8 |
|
|
|
|
|
|
|
|
|
h |
| 2021 |
WHO |
1,4 |
|
|
|
|
|
|
|
|
|
i |
Reference notes
a Medical Schemes 2020.109
b Medical Schemes 2021.110
c Medical schemes 2022.48
d DHB 2022/23.21
e Stats SA GHS 2021.111
f Stats SA GHS 2022.34
g World Health Statistics 2021.112
h World Health Statistics 2022.113
i World Health Statistics 2023.24
Definitions
• Claims ratio: Percentage of member contributions that have been utilised for the payment of benefits claimed by members of medical schemes, as opposed to allocation of contributions for non-health benefits and the building of reserves.
• Expenditure per patient day equivalent (district hospitals) [Rand (real prices)]: Average cost per patient per day seen in a hospital (expressed as Rand per patient day equivalent).
• Medical scheme beneficiaries [Number]: Number of medical scheme beneficiaries, as reported by the Medical Schemes Council.
• Medical scheme coverage [Percentage]: Proportion of population covered by medical schemes.
• Pensioner ratio [Percentage]: Proportion of members of medical schemes who are 65 years or older, in registered medical schemes.
• Proportion of population with large household expenditures on health as a share of total household expenditure or income [Percentage]: Proportion of population (%) with total household expenditures on health > 10% and > 25% of total household expenditure or income.
• Provincial & LG District Health Services expenditure per capita (uninsured) [Rand (real prices)]: Provincial expenditure on District Health Services (all sub-programmes except 2.8 Coroner services) plus net local government expenditure on PHC per uninsured population.
• Provincial & LG PHC expenditure per capita (uninsured) [Rand (real prices)]: Provincial expenditure on sub-programmes of DHS (2.2 - 2.7) plus net local government expenditure on PHC per uninsured population.
• Provincial & LG PHC expenditure per PHC headcount [Rand (real prices)]: Provincial expenditure on sub-programmes of DHS (2.2 - 2.7) plus net local government expenditure on PHC divided by PHC headcount from webDHIS.
• Total net official development assistance to medical research and basic health sectors per capita (US$), by recipient country.
Conclusion and recommendations
As South Africa strives to become more data driven and evidence informed in its healthcare decision making, improving information systems and data quality remain key objectives. Given that the majority of the existing information systems are still manual, the dangers of transcribing errors, as often observed by the Auditor General, necessitate more rigorous data quality and verification processes at all levels of the system.
Monitoring and evaluation (M&E) processes need strengthening at all levels of the health system. These processes should move away from simply tracking target achievement in a linear, mechanistic manner, towards ‘deeper dives’ that incorporate not only routinely collected data, but also research evidence and lived experience; processes that include a broader range of participants to enrich the analysis with different perspectives. These are critical procedures to rectify as South Africa seeks to track the health system’s performance in an integrated manner, better informing priority setting and decision making.
The National Health Insurance Act114 envisions better integration of the public and private sectors into a single health system, making obtaining and combining data from both sectors even more important. Governance systems that enable this must also be prioritised.
Despite South Africa’s high cancer incidence rate, the availability of reliable and up-to-date cancer data remains insufficient. This data gap poses significant challenges to effective cancer monitoring, policy formulation, and resource allocation. The National Cancer Registry (NCR), which serves as the primary repository for cancer data in the country, plays a crucial role in tracking the burden of cancer and evaluating patient outcomes. However, the registry currently faces limitations in data collection, coverage, and timeliness, which impede its ability to provide a comprehensive picture of the national cancer landscape.
Prioritising the enhancement and support of the NCR is critical not only for accurate tracking of cancer incidence and prevalence but also for generating detailed insights into cancer risk factors, survival rates, and the social, economic, and environmental determinants of cancer mortality. Enhanced data collection and reporting mechanisms would enable more precise identification of high-risk populations and regions, facilitating targeted public health interventions and tailored treatment strategies. Furthermore, robust cancer data can inform the development of prevention programmes, early detection initiatives, and evidence-based policy decisions aimed at reducing cancer disparities across different demographic groups.
In addition, strengthening the NCR will contribute to better understanding the impact of emerging trends, such as the rise in NCDs, the intersection of HIV/AIDS and cancer, and the influence of lifestyle changes on cancer patterns. Comprehensive, high-quality data is essential for evaluating the effectiveness of ongoing cancer control efforts and for guiding future research and funding priorities. By investing in the NCR and addressing the current data limitations, South Africa can significantly improve its ability to monitor and combat the growing cancer burden, ultimately leading to better health outcomes for its population.
Acknowledgements
This paper is a result of years’ worth of combined efforts at all levels of the health system. We would like to acknowledge the National Department of Health for the use of data from the web-based District Health Information System and National Treasury for the finance and human resources data. We would particularly like to acknowledge the work done on this section of the Review over the years by Candy Day. We also appreciate the valuable input received from the reviewers and thank them for their time.