Introduction
Occupational science is an inter-disciplinary field dedicated to the study of human occupation and is appropriate to various contexts such as public health, education and workplace wellness. Occupations are broadly defined as the activities in which people engage that occupy their time and bring meaning to their lives.1,2 These activities can range from daily routines and self-care tasks, to work, leisure and social participation, and are necessary not only for survival but also for personal fulfilment and societal participation. In occupational science, the concepts of ‘doing’, ‘being’, ‘becoming’, and ‘belonging’ are crucial to understanding human engagement and participation in daily activities.1
‘Doing’ refers to the activities and tasks in which people engage as part of their daily lives. The term encompasses everything from basic self-care routines to complex professional duties. It is important to note that engaging in meaningful activities is essential for physical and mental health, and helps individuals to express themselves and achieve their goals.2 ‘Being’ is about the experience of existing and living authentically in the moment. It involves reflection, introspection, and mindfulness, emphasising the importance of personal identity, self-awareness, and the intrinsic value of simply ‘being’ rather than constantly ‘doing’.2–4 ‘Becoming’ focuses on growth and development, both personally and professionally, and encompasses the process of evolving and reaching one’s potential.2–4 It highlights the dynamic nature of human life, emphasising change, aspiration and future possibilities. ‘Belonging’ involves the sense of being part of a community or social group, and is therefore about social inclusion, connectedness, and the relationships that provide support and identity.5 Feeling a sense of belonging is crucial for mental well-being, as it provides individuals with support networks and a sense of purpose and identity within a larger community. These concepts collectively help occupational scientists and therapists to understand how people engage with the world and how their activities, identities, growth and social connections contribute to their overall health and well-being.
In occupational science, situations where individuals or groups are denied the opportunity to engage in meaningful occupations result in negative impacts on health and well-being and are referred to as constituting occupational injustice.6 Occupational injustice manifests itself in various ways, depending on the impact of external and internal factors on individuals’ abilities to engage in meaningful and balanced occupations. For example, occupational alienation occurs when there is an experience of isolation, disconnection, or a lack of meaning in one’s activities, often due to repetitive, monotonous tasks or a mismatch between the individual’s values and the activities in which they engage.6 Occupational deprivation, on the other hand, is the state of being unable to engage in meaningful occupations over an extended period due to external restrictions such as social, economic, environmental or political factors.7 Finally, occupational imbalance refers to a disproportionate allocation of time and energy to different activities, leading to an over-emphasis on some occupations at the expense of others, which can negatively affect health and well-being.6 In addressing occupational injustice, effort must be made to address the equitable opportunities and resources required for individuals to participate in meaningful occupations, highlighting issues of social justice.
Occupational justice is a concept that foregrounds the rights of individuals to participate in meaningful activities and roles within society.8 Furthermore, occupational justice is the belief that everyone should have the opportunity to participate in occupations (activities) that are meaningful to them and contribute to their well-being, irrespective of socio-economic status, disability, or other environmental barriers.8 Additionally, occupational justice recognises that societal structures and systems can create inequalities that limit individuals’ abilities to participate fully in daily life activities. These inequalities can manifest in various forms, such as discrimination, poverty, disability, or lack of access to resources.
Healthcare workers can thus work to promote occupational justice by advocating for equitable opportunities and linking individuals to appropriate resources for them to engage in occupations (activities) that promote health, well-being, and participation in society. This may involve addressing barriers to participation, advocating for policy changes, and empowering individuals to advocate for their own rights. The core principles of occupational justice centre on empowerment, where individuals and communities should be able to make choices about their activities; inclusion, which ensures that all individuals can engage in a variety of occupations; and access, by removing barriers that prevent participation in meaningful activities.
The underpinning principles of occupational justice support a new way of thinking about mental health interventions, and such justice lends itself to relying on multi-sectoral and inter-disciplinary stakeholders as change agents working collaboratively towards enhancing societal well-being.
The benefits of framing mental health around the principles of occupational justice are well demonstrated by a framework developed by the Western Cape Department of Health and Wellness (WCDoHW) for the expansion of Psychosocial Rehabilitation Services (PSR) in response to increasing mental health service pressures. Initiated in 2023, this framework aims to address the needs of individuals across the mental health continuum, including people with mental disorders, while also promoting mental well-being across the broader population.
Psychosocial rehabilitation is a therapeutic approach that aims to promote personal recovery, successful community integration, and acceptable quality of life for persons who have a mental disorder.9 Moreover, the wide range of PSR services and support is collaborative, person-centred and individualised, with the focus on helping people to develop the skills and access the resources needed to increase their capacity to develop agency and be successful and satisfied in their living, working, learning, and social environments.9
This paper outlines the process employed by the WCDoHW to develop a PSR framework and illustrates the benefits of framing mental health around the principles of occupational justice.2
Case description
The concept of PSR is not new to the Western Cape. The need for PSR services in the province first emerged due to changes in the National Health Policy of South Africa after the first democratic election in 1994, which focused on the de-institutionalisation of mental health care users and the facilitation of re-integration into their communities. At the time, there was a paucity of approaches that were suitable for providing PSR in the South African context. The WCDoHW therefore considered building on available international approaches. In 1998, the National Department of Health (NDoH) reached out internationally, requesting appropriate support. The NDoH partnered with the Stichting Overlegorgaan Geestelijkie Gezondheidszorg (SOGG) in the Netherlands for technical support to develop a PSR policy framework. It was agreed to build the necessary capacity among clinicians to ensure sustainability.
Various projects were initiated by the participants during the training programme. These projects continued at regional (rural and metropolitan) and institutional levels, with some support from the Western Cape Provincial Mental Health Programme Managers. In Rural Health Services, the mental health nurses who had been trained, co-ordinated the implementation of PSR groups and incorporated them into mental health services in the Garden Route and West Coast Districts, specifically. A non-profit organisation (NPO) in the Cape Metro was contracted by the WCDoHW to facilitate PSR in the community in 2004. Twenty-six groups were established across the metro and served approximately 250 clients per annum.
In 2016, a situational analysis of the existing PSR service in the Cape Metro was conducted. A significant finding was that the 26 groups served as maintenance and support groups for those with chronic mental illness, but did not offer sufficient functional enhancement, recovery, and effective re-integration into the community.10 The key recommendation was to revisit the PSR model and adapt the interventions to suit the recovery needs of clients who required varying levels of support.
In 2021, the Medium-Term Expenditure Committee11 (MTEC) acknowledged that poor mental health is not restricted to those with mental illness, but that anyone can experience poor mental health when faced with stressors that become overwhelming. This increased pressure, which was exacerbated by the impacts of COVID-19, further highlighted the need for the redesign of mental health services. Consensus was reached in the Western Cape Government (WCG) that to address the mental health needs of people, a whole-of-society approach (WoSA) and whole-of-government approach (WoGA)11 were required. It was agreed that mental health care should be addressed through evidence-based research and engagement with the political, economic, and ethical dimensions of the choices in mental health care, and that it was essential to strive for equity in mental health care provision. The WCG acknowledged that the integration of mental health into general health care is a key factor to improving mental health services, and that mental health cannot be separated from physical health.11,12
Mental health thus emerged as a priority for the WCG and a decision was made to prioritise mental health care across all departments.12 Through such prioritisation, additional funding was obtained in 2023 to strengthen and expand mental health care services at the Primary Health Care (PHC) level. These additional funds enabled the WCDoHW to expand existing PSR services for the inclusion of all people who require psychosocial support across the mental health continuum.
Mental health is defined as a state of well-being in which every individual realises their potential, can cope with the normal stresses of life, can work productively, and can contribute to their community.13 Moreover, mental health occurs across a continuum between mental well-being and mental illness.14 Depending on the circumstances of any individual at any time, their position on the continuum may shift as their situation improves or deteriorates. Therefore, mental health services must address mental health needs across the mental health continuum through the provision of promotion, prevention, curative, rehabilitation, and palliation services.
Method
Consultative workshops were held with healthcare workers from across the care continuum to identify service gaps and opportunities for expanding PSR services. Thematic analysis of the feedback informed the development of the expanded framework.
Although occupational justice was not part of the initial approach, engagement with healthcare workers during the first workshop revealed the need for a clear theoretical foundation to underpin the emerging model. Based on our thematic analysis of the insights from that session, the development team made a conscious decision to adopt occupational science as the armature to form the framework, with a strong emphasis on occupational justice as a key principle. This decision was based on the understanding that occupational justice is already commonly applied in healthcare settings by occupational therapists to inform a range of interventions, including PSR and support services. This concept was then introduced in subsequent workshops where it was used in the discussions to guide the continued development and refinement of the PSR framework and its associated interventions as it aligns with occupational justice.
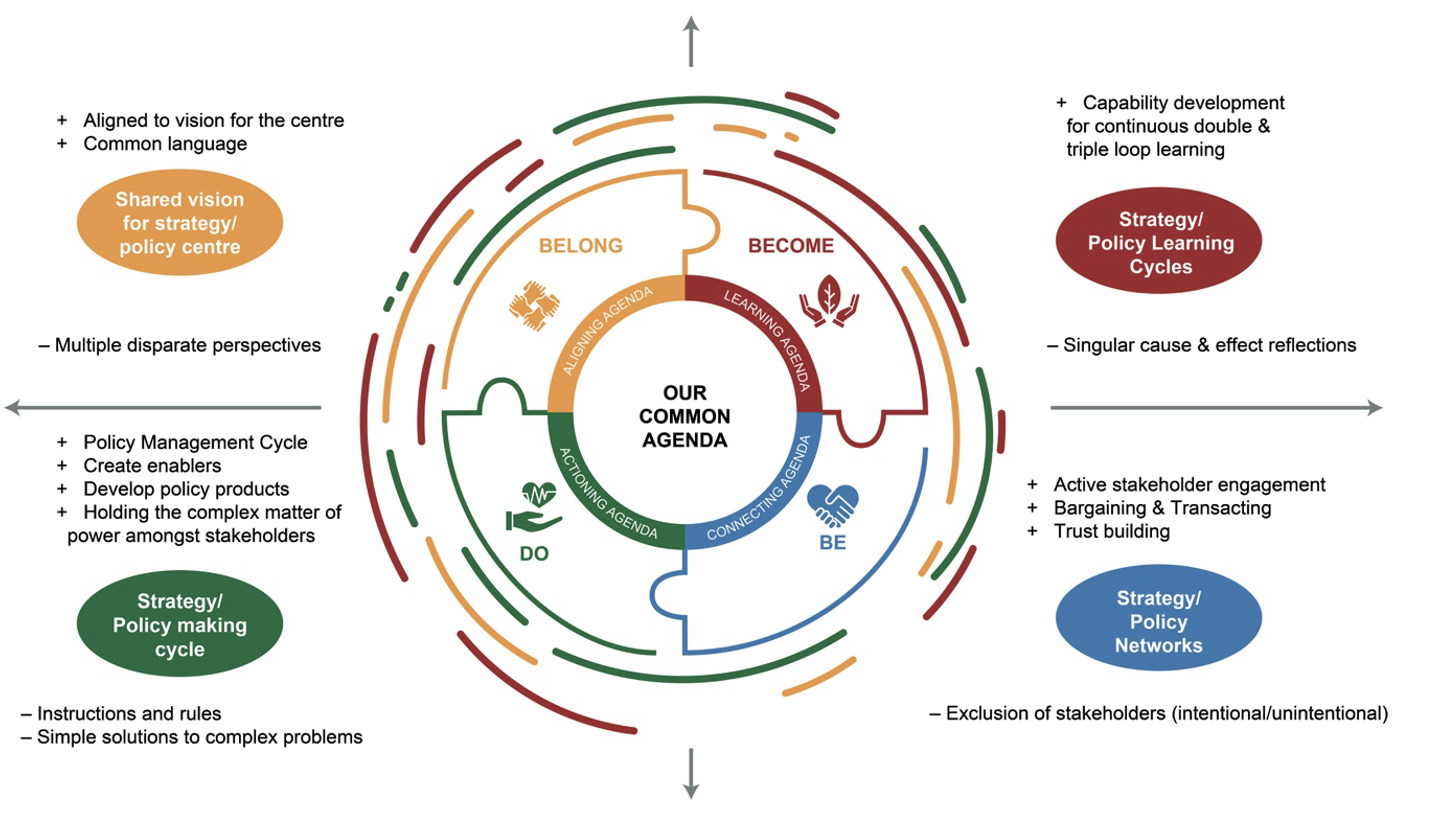
The developers of the framework made use of the WCDoHW common agenda of ‘Doing, Being, Becoming and Belonging’15 (Figure 1) to guide the process.
The WCDoHW common agenda is informed by the ‘CALM’ approach for collaborative innovation, which comprises four key agendas, namely: connecting, aligning, learning, and making/actioning.16 It emphasises a balanced, thoughtful, and sustainable approach to introducing and managing change within an organisation, and integrates the principles of purposeful innovation, incremental change, sustainability, person-centred design, collaboration, and continuous learning.16 By adopting the CALM approach, the developers were able to create a balanced process that fosters creativity, stability, and long-term success. The specific agendas of the approach are described as follows.
Connecting
The ‘connecting’ agenda is centred on building trusting connections across many boundaries.16 For this project, a task team was established consisting of members with various levels of PSR expertise, as well as innovative thinkers and members who encouraged the group to be aspirational. The team facilitated several consultative workshops where a range of participants, including healthcare workers from across the healthcare continuum, the NPO sector, various government departments, and service users, provided inputs on service gaps and the scope for PSR services. This enhanced idea-generation from diverse perspectives and built a strong support network for innovative initiatives.
Aligning
The ‘aligning’ agenda refers to alignment around a clear and deeply shared intention for working together.16 The task team ensured that there was alignment with existing departmental strategies such as Healthcare 2030,17 the Make Every Contact Count (MECC) counselling strategy,18 differentiated models of care (DMoC),19 community-orientated primary care (COPC),20 and the overarching transversal mental well-being strategy. Additionally, the team ensured that there was alignment with occupational science, and occupational justice in particular.2 Such alignment ensured that innovative efforts were in harmony with the WCDoHW mission, values, and strategic goals, and enabled stakeholders to focus on the innovation at hand, thus creating buy-in.
Learning
The ‘learning’ agenda is designed to gain a deep understanding of the system and the human experience within it.16 It promotes continuous learning and adaptability within the organisation by implementing feedback loops and iterative development processes. Learning encourages increased agility and responsiveness to changes and the development of a growth mindset among stakeholders. The feedback from each consultative workshop was analysed into themes and used to inform development of the framework. This was an iterative process, and changes were made after every workshop based on the input and feedback from the various stakeholders. A key insight that influenced the final framework was the need for a theoretical framework, i.e. occupational justice, as well as the need to prioritise community and employee resilience to give full effect to the overall bouquet of psychosocial interventions.
Making
The ‘making’ agenda refers to building and testing tangible solutions and bringing them to scale.16 The expanded framework for PSR support services incorporated clear processes for moving from ideation to implementation were established. It also provided guidance on resource allocation to ensure that there would be sufficient support to facilitate the translation of ideas into tangible outcomes through systematic development and implementation.
Results
The framework for the expansion of PSR and support services was subsequently developed with a particular focus on occupational justice as a protective factor to enhance mental health and well-being.2 The framework serves to redefine psychosocial interventions in the Western Cape by offering a deeper understanding of how mental health occurs on a continuum and how the principles of PSR can be used to address the entire continuum. For this reason, the PSR principles should be applied more broadly than mental disorders and address several other factors that could affect overall health and well-being negatively such as life transitions (e.g. retirement; becoming a parent), adjusting to major life events (e.g. divorce; loss of a loved one), physical health challenges (e.g. HIV; TB; long-term medical conditions; disability), substance use, career and education goals, and social isolation and loneliness (e.g. stigma; ageing).
The objectives of this framework for expansion of PSR support services are to provide:
-
insight on the mental health support needs across the mental health continuum; and
-
a framework for staff to use in developing psychosocial interventions that are resource- and context-specific.
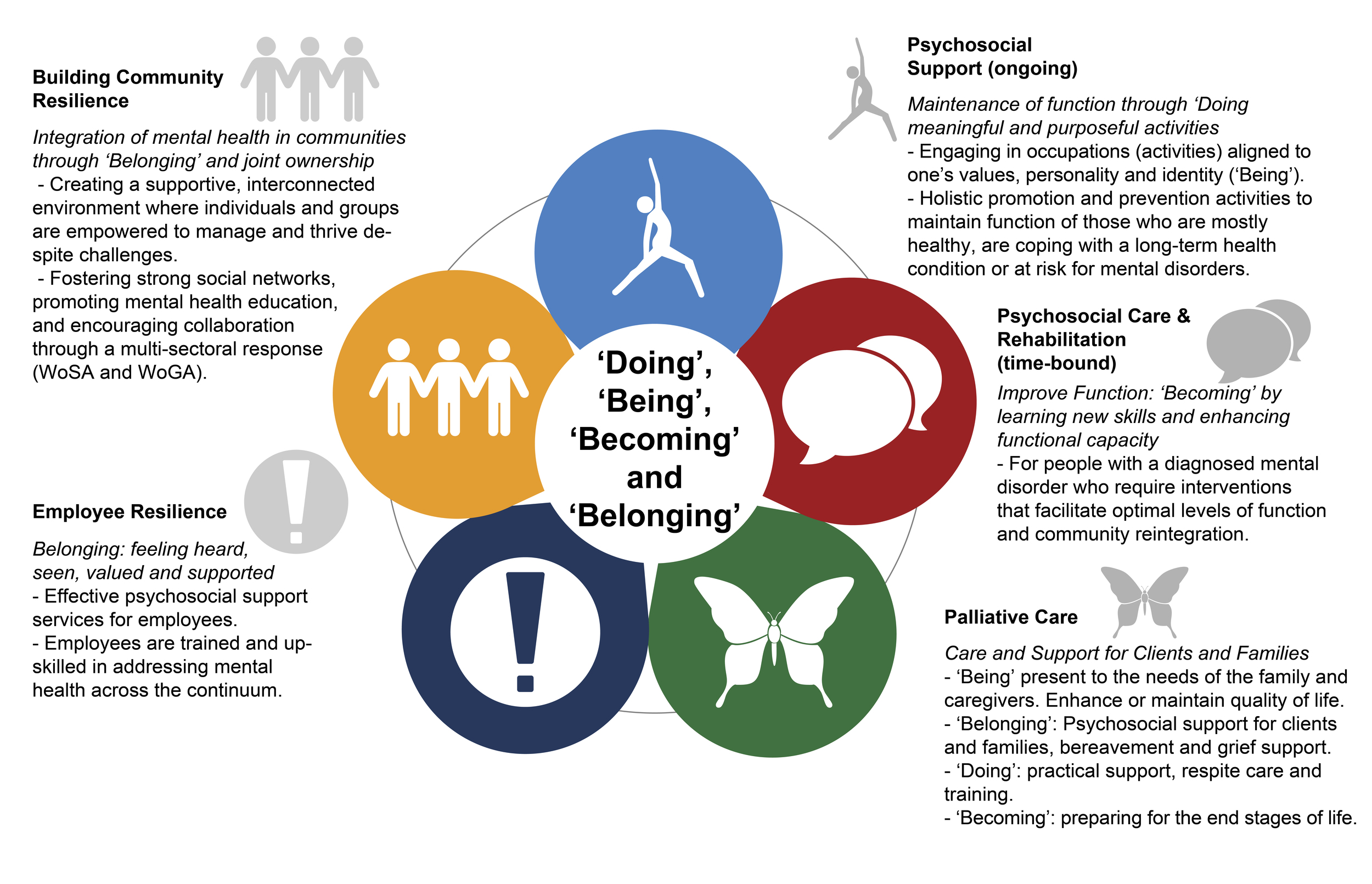
The framework consists of a bouquet of psychosocial interventions with five key components: (1) building community resilience; (2) psychosocial support; (3) psychosocial care and rehabilitation; (4) palliative care; and (5) employee resilience, as illustrated in Figure 2.
Building community resilience
Building community resilience to support mental health requires a multi-faceted approach that entails strengthening social networks, promoting access to mental health services, increasing education and awareness, and creating environments that support social prescribing. Occupational justice underpins this approach by advocating for every individual’s right to engage in meaningful daily activities, regardless of social, economic, or health-related barriers.6 By implementing these strategies, communities can enhance provision of support for the mental well-being of their members. WoSA and WoGA are key elements of this component, and clear referral pathways are established.
Multi-sectoral responses are needed to promote equitable access to services and to utilise the resources within a community. Additionally, this component aims to strengthen understanding of and support for mental health at community level, creating a supportive environment where clients with mental disorders can re-integrate into their communities more easily. This component also aims to address the stigma associated with poor mental health and encourages community participation, thus lending itself to a COPC20 approach. This involves co-ordinating an integrated approach to health and well-being with multiple stakeholders within a defined community/geographical area. COPC addresses the major health needs and challenges of the community served, tackles social determinants of health, and proactively focuses on the promotion of health and the prevention of disease.
Psychosocial support
Psychosocial support focuses on holistic promotion and prevention activities as well as occupational enrichment activities to maintain the functioning of those who are mostly healthy or at risk for mental illness. Through the lens of occupational justice, this component ensures that individuals have equitable opportunities to engage in meaningful roles and routines that support identity, purpose and well-being. PSR principles such as skills development, social support and empowerment are adapted to support clients in improving wellness, learning how to navigate life and relationship changes, dealing with health diagnoses, and/ or improving their overall outlook on life. Participation is voluntary, and the support provided is through a multi-disciplinary approach across all government sectors. Persons with a diagnosed mental disorder, who are clinically stable, may also benefit from psychosocial support to help maintain their function and prevent relapse. Psychosocial support interventions can be graded at the discretion of the therapist to meet the needs and level of functioning of the participants. Additionally, interventions can take place in the form of a club as a differentiated model of care.19 Psychosocial support interventions serve as an opportunity to make every contact count,18 which is aimed at early identification of risk through screening and early intervention in the form of brief modalities and appropriate referrals.17
Psychosocial care and rehabilitation
This component addresses clinical care and rehabilitation for individuals with diagnosed mental disorders who experience functional impairment. Interventions aim to improve functioning, support recovery, and enable meaningful occupational engagement ─ these being the key tenets of occupational justice. Supporting individuals to regain control over their lives and re-integrate into their communities affirms their right to participate fully in society, despite mental health challenges. Interventions may include skills training, group or individual therapy, and empowerment activities tailored to the person’s goals and needs. These interventions may have a set timeframe, and as functioning improves, individuals may transition to psychosocial support services to maintain gains. The integration of occupational justice ensures that rehabilitation is not limited to symptom reduction but also supports re-engagement in personally meaningful roles and social participation.
Palliative care
Palliative care within the PSR framework extends beyond symptom management to include comprehensive psychosocial support for clients and their families. Such care supports understanding of medical diagnoses, enhances quality of life, and ensures that individuals can continue to participate in valued roles for as long as possible. Grounded in occupational justice, this approach promotes dignity, choice, and inclusion in end-of-life care, ensuring that clients are supported in maintaining their occupational identity and daily routines. Family capacitation and grief counselling extend the focus of care to relational well-being, recognising the broader social and occupational systems in which people live and die.
Employee resilience
This component recognises the need to uphold occupational justice for healthcare workers by ensuring fair and supportive work environments that enable meaningful participation, professional development, and emotional well-being. This is a critical component of the PSR framework and is aimed at assisting staff in maintaining their mental health or seeking help when needed. Access to employee wellness programmes should be encouraged, and a healthy work environment where staff feel heard, seen, valued and supported should be created. In the context of staff wellness, the work environment is the community which requires focus. In addition, appropriate training should be available to support and capacitate staff to address mental health and intervene appropriately within their contexts. Furthermore, sufficient training should be available for all healthcare workers to empower the workforce with a deeper understanding of mental health and their role in supporting their clients. By promoting a healthy work environment and respecting the occupational rights of employees, this component helps to sustain the workforce and improve service quality.
Table 1 elaborates on the components of the PSR bouquet of psychosocial support with examples of role-players, target audiences, and possible activities.
Discussion
As the focus of the framework for expansion of PSR support services, occupational justice underpins psychosocial rehabilitation effectively because it addresses how meaningful daily activities (occupations) support health, identity and well-being. Occupational justice aligns with the person-centred, strengths-based approach of psychosocial rehabilitation by promoting individual agency, community integration, and functional recovery. Its holistic and evidence-informed perspective helps in the design of interventions that support real-life participation and long-term recovery. By examining the complexities of occupational justice, researchers and practitioners can develop more effective strategies to enhance individuals’ quality of life across various contexts and stages of development.
Key to this understanding of occupational engagement is the concept of occupational consciousness. According to Ramugondo,21 occupational consciousness refers to the awareness and understanding of how occupational choices and engagements are influenced by broader social, cultural, economic, and political factors. It involves recognising the ways in which these factors shape opportunities for meaningful occupation and the potential for occupational injustice. This concept emphasises the importance of understanding the broader context in which occupational activities occur and highlights the role of power dynamics and systemic structures in shaping occupational experiences. For example, social conditions such as unemployment, poverty, substance misuse and high levels of violence in the Western Cape have been proven to negatively affect mental health and the ability of people to engage in meaningful activities that promote health and well-being. These structural barriers within communities foster occupational injustice and highlight the need for innovative approaches for the provision of mental health services and needed support.
The expanded framework for psychosocial support aims to facilitate occupational justice by providing opportunities for participation in meaningful occupations that promote a sense of purpose, achievement, and self-worth. Engaging in activities that align with personal values and interests can significantly boost mental health.8 In addition, activities that individuals find enjoyable and fulfilling can reduce stress and anxiety, providing a mental break from daily pressures.6,22 The framework also promotes social inclusion and support by encouraging community involvement through engaging in communal activities, fostering social connections, and reducing feelings of isolation and loneliness which are significant risk factors for mental health concerns.8 Social participation in group activities can create support networks that offer emotional and practical support, thereby enhancing resilience and coping strategies.4
Additionally, the framework addresses inequities by advocating for equitable access to resources and opportunities, which is crucial for mental health. Lack of access to meaningful occupations can lead to feelings of helplessness and depression.7 Most importantly, the framework aims to empower staff and clients to be attentive to human rights issues so that they can promote self-determination, gain a sense of control over their lives, and be agents of social transformation ─ all of which are essential for mental well-being.23
Promoting occupational justice is also critical for building community resilience. By ensuring inclusive employment opportunities, access to education, community engagement, inclusive environments, and mental health support, communities can empower individuals to contribute meaningfully and sustain their well-being. These strategies not only enhance individual quality of life, but also strengthen the collective resilience of communities.22
The implementation of the framework is co-ordinated by an inter-disciplinary team of providers, i.e. occupational therapists, psychologists, social workers, doctors, nurses and other relevant professionals and non-professional cadres to deliver comprehensive care. The inter-disciplinary team can work with individuals, groups, or communities to identify person-centred needs and tailor interventions that support mental health, address barriers to participation, and are in line with the specific needs, preferences, and goals of each client. Practical applications in psychosocial support include developing community-based programmes that involve leveraging community resources such as local support groups, recreational facilities, and educational programmes that provide opportunities for all individuals to engage in meaningful activities. Collaboration with multi-sectoral stakeholders such as individuals with disabilities, refugees, and those living in poverty is essential to ensure accessibility to marginalised populations.
It is important to continuously evaluate and adjust care plans to respond to changes in the patients’ conditions and circumstances. Interventions can include lifestyle redesign, self-management support, health education, treatment literacy, peer support, skills training, sport and recreation, and environmental modifications to facilitate active participation in the community.
The implementation of PSR services highlights potential challenges such as co-ordinating inter-disciplinary teams, resource limitations, inequitable access, and the need for ongoing monitoring. Lessons learnt include the value of person-centred, community-based care, the effectiveness of flexible and responsive interventions, and the power of peer support and skills development in promoting recovery. A key insight is the importance of building both employee and community resilience to sustain care and adapt to changing needs. PSR services are scalable through modular interventions, task-sharing, and use of existing infrastructure. The framework is replicable across diverse settings when rooted in cultural relevance, community participation, and multi-sectoral collaboration.
Recommendations
The mental health burden in the Western Cape continues to increase and worsened significantly during the COVID-19 pandemic, which exacerbated the drivers for poor mental health, resulting in increased pressure across the health system.11 Innovative approaches for providing mental health services and support are therefore required. Additionally, the protection and promotion of mental health and overall well-being in the general population has been identified as crucial for maintaining the functioning of those who are healthy or at risk for mental disorders.5
The following recommendations should be considered for strengthening psychosocial support and rehabilitation:
-
Enhance transitional mental health care: Strengthen transitional care services to ensure continuity and integration across levels of care. Expanding the implementation of the PSR framework will optimise both physical and psychosocial outcomes for clients by embedding PSR services within the health system.
-
Develop workforce training and communication plans: Establish comprehensive training and communication strategies to prepare and empower the health workforce for effective implementation of the PSR framework. This should include capacity-building initiatives, supportive supervision, and ongoing professional development.
-
Promote inclusive policy development: Advocate for and develop inclusive policies that actively dismantle barriers to participation in meaningful occupations by individuals with mental health conditions. These policies should address structural, environmental and attitudinal barriers.
-
Ensure inclusive infrastructure and workplace accommodation: Improve access to inclusive recreational facilities and ensure that workplace environments accommodate the needs of individuals with mental health challenges and disabilities. This includes physical accessibility, supportive policies, and flexible work practices.
-
Implement transversal, systemic policies for social inclusion: Introduce and strengthen transversal policies that promote systemic change across sectors to reduce exclusion and enhance participation. Areas for policy development include:
-
Community and public safety promotion
-
Accessible and reliable public transportation
-
Affordable and inclusive childcare services
-
Availability of adaptive and assistive equipment for individuals with disabilities
-
-
Support advocacy and community-based initiatives: Strengthen advocacy efforts to reduce stigma, raise awareness, and promote the importance of psychosocial care across the mental health continuum. Key focus areas include:
-
Resource mapping and referral pathway development
-
Community mobilisation and capacity-building
-
Life course approaches to mental health promotion
-
Prevention and early intervention strategies
-
Conclusion
The framework for the expansion of psychosocial rehabilitation support relies on multi-sectoral and inter-disciplinary stakeholders as change agents working collaboratively towards enhancing societal well-being. By integrating occupational justice into mental health and psychosocial support strategies, more inclusive and supportive environments that provide people with diverse choices can be created, thereby enhancing well-being and quality of life for all individuals and communities. Moreover, such integration enables communities to provide robust psychosocial support that promotes mental health, fosters social connections, and ensures that all individuals can engage in meaningful and purposeful occupations.