Introduction
The first case of SARS-CoV-2 infection was reported in Wuhan, China, in December 2019. The ensuing pandemic affected most countries severely, with the burden of COVID-19 disease and accompanying lockdown regulations impacting on the provision of routine and essential health services. South Africa was no exception, given its pre-existing quadruple burden of diseases, including HIV and tuberculosis; non-communicable diseases (mainly hypertension and diabetes); suboptimal maternal and child health; and violence/injury.1
Providing continuity of healthcare services in an already stretched healthcare system is challenging, particularly during a pandemic. South Africa reorganised its healthcare services by increasing medical and laboratory capacity and building field hospitals – all in anticipation of a rapid increase in number of adult COVID-19 cases. Additionally, the country implemented a level-5 lockdown in March 2020, which prohibited non-essential economic activity, limited movement of people outside their homes, and restricted availability of transport for commuters. Four distinct COVID-19 waves ensued between March 2020 and March 2022, leading to the enforcement of several levels of lockdown restrictions. Despite public-health interventions to curb the spread of SARS-CoV-2, routine and emergency healthcare services needed to continue to avoid collateral morbidity and mortality, resulting in major strains on the healthcare system.
International research has highlighted widespread and significant impacts of the COVID-19 pandemic on the provision and utilisation of healthcare services, especially those related to maternal, newborn, child and women’s health (MNCWH).2 In attempting to understand the impact on the healthcare system it is insufficient to rely solely on hospital-based studies, as disease burden may shift within the context of severely constrained pandemic environments. The Tshwane Health District has the same geographical boundaries as that of the Tshwane metropolitan municipality. It is a largely urban district in the Gauteng Province of South Africa with a population of 3 552 452 people, and a total surface area of 6 345 km², making it the third-largest municipality in the world by surface area.3 Primary health care (PHC) facilities in Tshwane District provided continuous services during the pandemic as reported in district management meetings and personal communications with clinicians, with occasional short-term closures due to COVID-19-related prevention activities.
The research aim was to gain a better understanding of the effect of the COVID-19 pandemic on the uptake of routine MNCWH services in Tshwane District, rendered mainly at PHC facilities and district hospitals (public-sector facilities), as well as at community level and at schools/crèches.
Methods
As part of the observational Tshwane Maternal-Child COVID-19 study, routine data sources, including the District Health Information System (DHIS) and other district-based datasets, were analysed from April 2019 to March 2022, to describe the impact of the COVID-19 pandemic over the first four epidemic waves in Tshwane District.[1] The year pre-pandemic was used as baseline. Data elements and indicators included those relating to MNCWH (including reproductive health, termination of pregnancies, cervical cancer screening, clinical forensic medical services, obstetric care, and early infant HIV diagnosis), child health (including immunisations, Vitamin A, deworming, and school health), and COVID-19 surveillance (including cases, hospitalisations and deaths). Only a selection of data elements was included in this analysis due to the large number available; the current focus was on clinical and preventive services provided at public health facilities at different levels of care, together with services provided at schools and community level, in order to study the impact of the COVID-19 pandemic on broader maternal-child health service provision within these different contexts and settings. In-depth analysis of clinical care provided mostly at hospital level, and maternal-child outcomes (including morbidity and mortality rates), were not the focus of this particular study.
Data analysis included descriptive statistics, together with visual analysis of trends over time. Statistical investigation included testing of differences between data from the pre-pandemic year, as baseline, compared with results from the following two pandemic years (2020/2021 and 2021/2022), as per the National Department of Health’s financial years (from April to March of the following year). Shapiro Wilk’s test was used to determine if data were normally distributed, followed by inferential tests, including the independent t-test as well as the non-parametric alternative, the Mann-Whitney U test, to compare the pre-pandemic baseline results with those obtained in the two pandemic years. Additional investigations included paired comparisons, including the paired t-test and Wilcoxon signed-rank test, comparing the months of the baseline group with those from the pandemic years (2020/2021 and 2021/2022) to investigate changes over these periods. Significance tests were performed at 5% level of significance, and the analysis was performed using the statistical program R.4
Research permissions were obtained from the Ethics committees of the University of Pretoria and Sefako Makgatho Health Sciences University together with relevant provincial and district approvals.
Key findings
The Tshwane District COVID-19 pandemic followed a similar pattern to the rest of South Africa, with four distinct waves occurring between April 2020 and March 2022 (Figure 1).
Women’s health and reproductive services
Family planning
Utilisation of modern contraceptive methods to prevent unplanned pregnancies was measured using the composite indicator couple-year protection rate (CYPR). The year-on-year average CYPR was lower in 2020/2021 (40.8%) and 2021/2022 (37.0%), than in the pre-pandemic year when it was 46.8% (p=0.04; pre-pandemic versus pandemic period). The CYPR showed an annual decrease over the December summer vacation period. There was an additional sharp decrease in April 2020 to 18.6%, which corresponded with the first strict COVID-19 lockdown in South Africa (Figure 2).
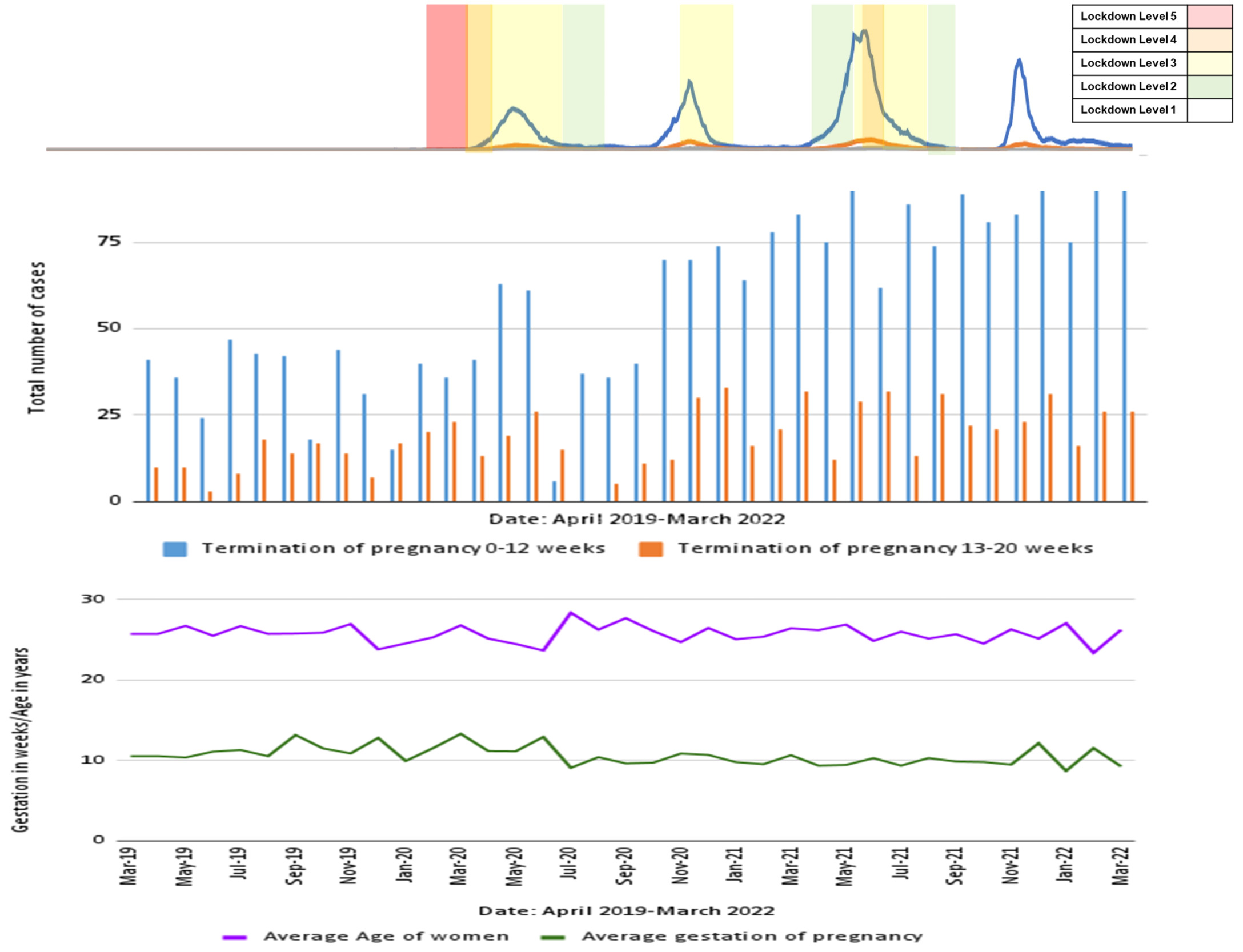
Termination of pregnancy services
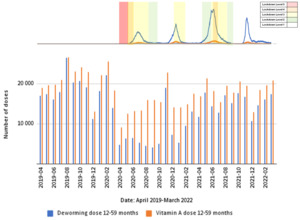
Termination of pregnancy (TOP) services in Tshwane District were mostly maintained despite an initial drop at the start of the pandemic and lockdown regulations; they increased again from March 2021 onwards (Figure 3). The average number of total TOPs was 508/month (pre-pandemic), 494/month (2020-2021), and 628/month (2021-2022) (p=0.1236 for total TOPs 2021-2022 versus pre-pandemic).
During the study period, Jubilee District Hospital, situated in Tshwane Sub-district 2, was the only site providing both first- and second-trimester TOP services in the entire sub-district and district respectively, and an important contributor to the district’s overall TOP numbers. Before September 2020, the hospital’s TOP clinic had two allocated clinicians, with only one trained to perform procedures. A new staff member was appointed in October 2020, with more staff added in 2022, increasing the capacity and therefore leading to a subsequent rise in the number of procedures performed and increasing the district’s overall TOP numbers (Figure 4). The TOP clinic register, a DHIS source document, showed that the average age of the women utilising the clinic’s service, and average gestation at time of TOP, which stabilised around 10 weeks’ gestation, were both not much affected by the pandemic or the local increase in service capacity.
Cervical cancer screening
There was a marked decrease in the monthly number of cervical cancer screenings, from an average of 5 455 samples/month (pre-pandemic), to 3 453/month (2020-2021), and with a nadir of 2 147 in July 2020 (Figure 5). There was a corresponding decrease in detection of high-grade precancerous cases from 3 609 cases/year (2019-2020), to 2 020 cases/year (2020-2021), and 2 041 cases/year (2021-2022).
This DHIS indicator changed in April 2020, from the number of cervical cancer screenings done in women above 30 years of age, to also include the number of cervical cancer screenings done for women living with HIV above 20 years of age. A discrepancy was noted when comparing the number of cervical cancer screenings captured on the DHIS and corresponding sample numbers received by the National Health Laboratory Service (NHLS), especially during the period from April 2020 to June 2020, which coincided with the strictest lockdown period (Figure 5).
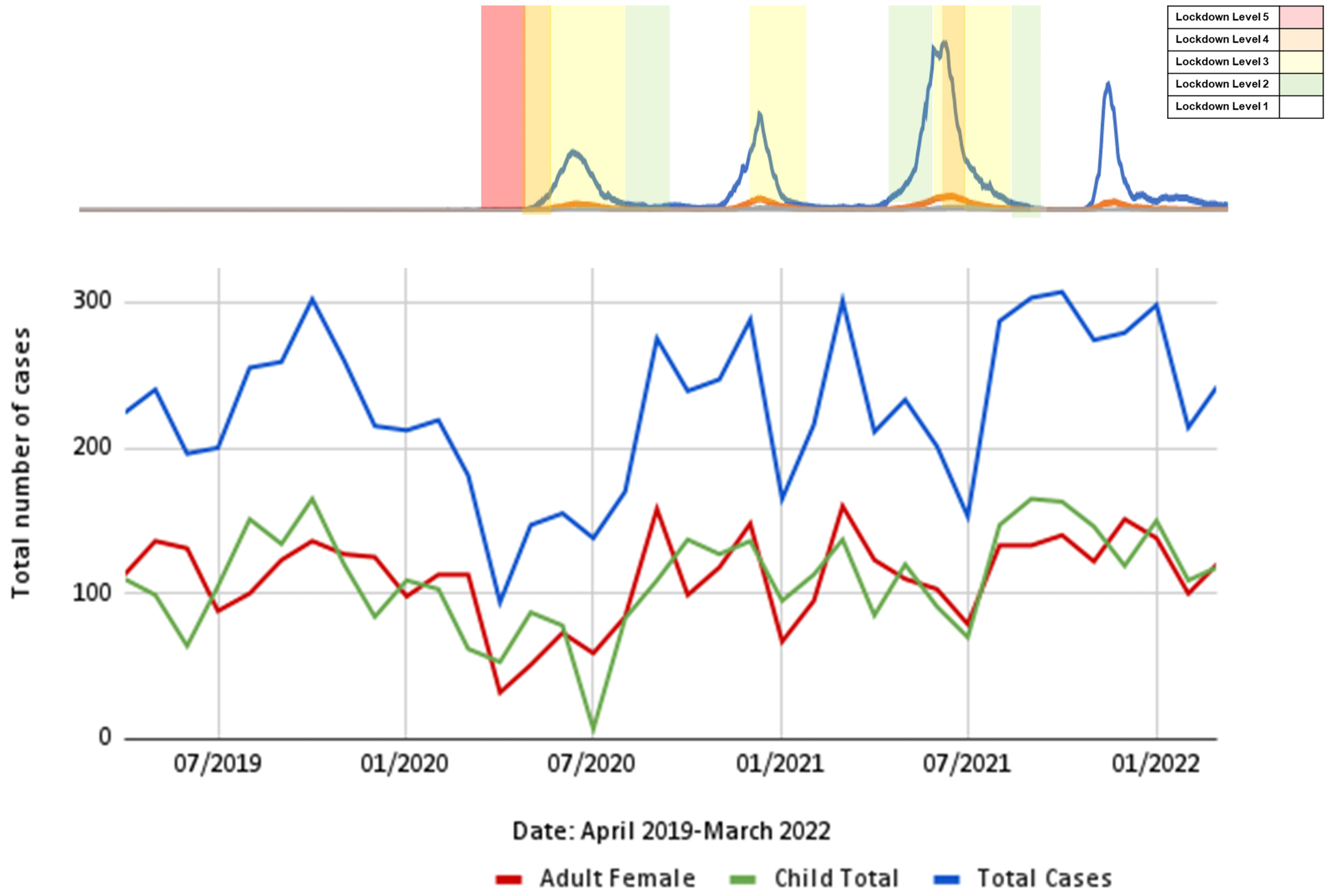
Forensic clinical services
The seven dedicated Clinical Forensic Medical Centres in Tshwane District manage survivors of crime (particularly sexual assault, domestic violence and child abuse), supporting judicial processes through evidence collection and provision of expert witnesses. The monthly total client numbers and subgroups of adult females and children seen for clinical consultations showed a sharp decline, from an average of 230/month (pre-pandemic) to 94 during April 2020, corresponding with the strict lockdown at the start of the pandemic, with subsequent stabilisation afterwards to pre-pandemic numbers (Figure 6).
Maternal and neonatal health
Antenatal care
Antenatal care provision was mostly maintained throughout the study period, despite some monthly variations, for instance in April 2020 (the first month of strict lockdown) (Figure 7). Overall, there were slight reductions in monthly numbers of first antenatal visits over the three-year period, with averages of 5 090/month (pre-pandemic), 4 875/month (2020-2021), and 4 754/month (2021-2022) (p=0.261 for total first antenatal visits 2021-2022 versus pre-pandemic).
It is further appreciable that the majority of pregnant women in Tshwane District booked for antenatal care before 20 weeks’ gestation (pre-pandemic average of 64.7%), and this was maintained throughout the pandemic period, with a slight decrease to 62.0% in 2020-2021, but with a subsequent increase to 66.4% in 2021-2022.
Deliveries and stillbirths
The average monthly number of in-facility deliveries was 4 786/month (pre-pandemic), 4 962/month (2020-2021), and 4 719/month (2021-2022), showing a reduction at the end of the study period (average of 4 554/month in the last six months) (Figure 8). The stillbirth numbers fluctuated, with average numbers of 98/month (pre-pandemic), 109/month (2020-2021), and 98/month (2021-2022), with two spikes noticeable in the first pandemic year – the first occurred just after the first COVID-19 wave, and the second more sustained peak stretched from the second to the third COVID-19 waves (p=0.045; 2020-2021 versus pre-pandemic).
Teenage pregnancies
The ‘delivery in 10 to 19 years in-facility rate’ indicator is used to monitor the percentage of in-facility deliveries in young women under 20 years of age. This indicator showed an increasing trend over the study period (Figure 9), with average monthly percentages increasing from 8.0% (pre-pandemic), to 8.7% (2020-2021), to 9.4% (2021-2022) (p=0.05 for pre-pandemic versus 2020-2021; p=0.03 for 2020-2021 versus 2021-2022).
Babies born prior to their mothers’ arrival at a health facility
The number of babies born before arrival (BBA) at a health facility gradually increased from 146/month (pre-pandemic), to 177/month (2020-2021), and 191/month (2021-2022) (p<0.001 for pre-pandemic versus 2021-2022) (Figure 10). This timing of the increase corresponded to restrictions on personal movement during the lockdown periods, with no trend reversal seen with easing of lockdown regulations. There was a marked peak in BBA numbers in July 2021 (n=236), just after the third and largest COVID-19 wave in the district.
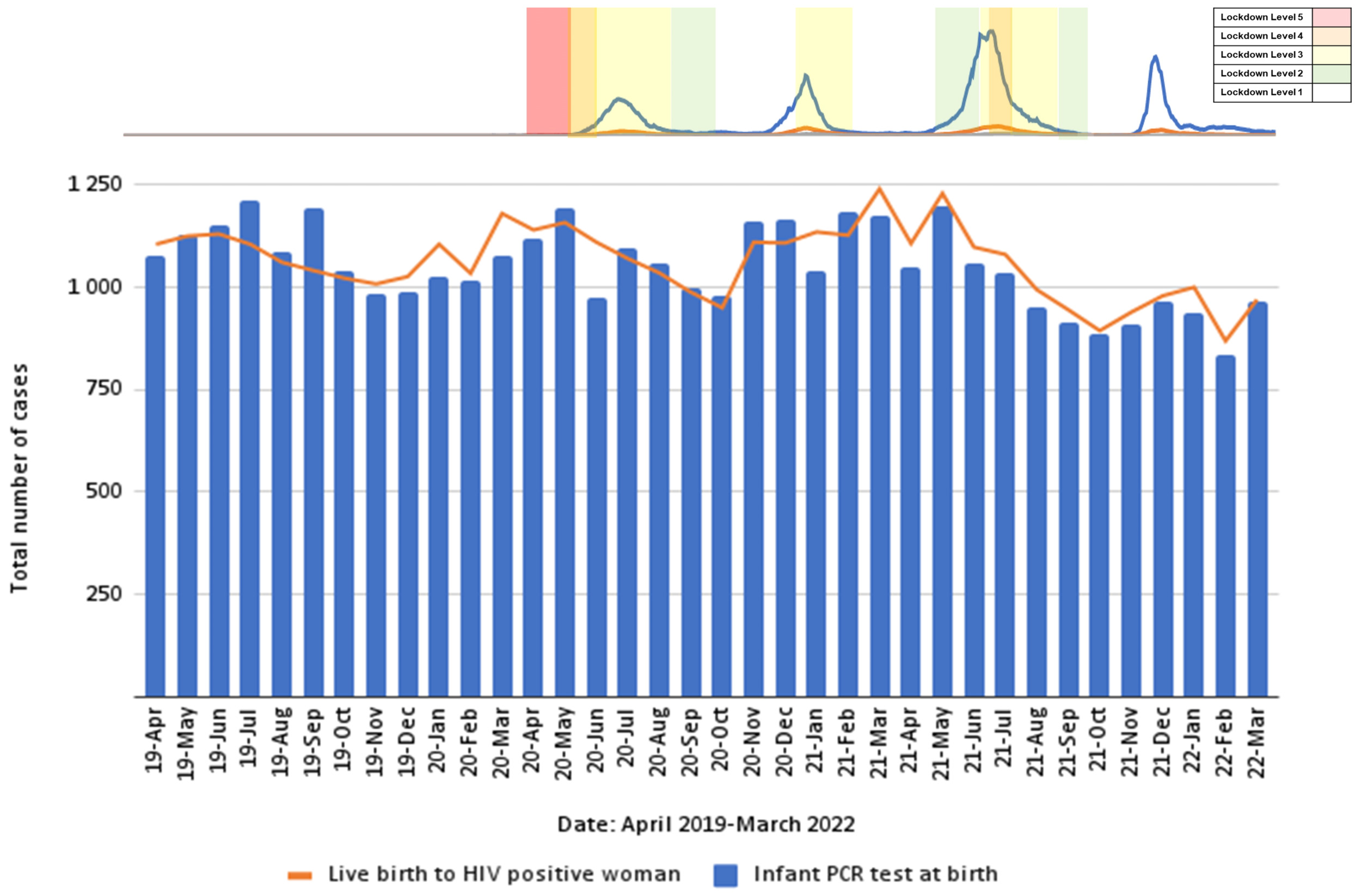
HIV programme
As a gauge for the robustness of the HIV programme to maintain MNCWH service coverage during the pandemic, the number of infant birth HIV Polymerase Chain Reaction (PCR) Reaction tests was compared with number of live births to HIV-positive women, as recorded in the DHIS (Figure 11). Data showed that the early infant diagnosis programme was well maintained, in terms of infant birth testing. There was a decrease in number of recorded live births to women living with HIV in the last year of study, leading to a corresponding decrease in number of infant birth PCR tests.
Child health
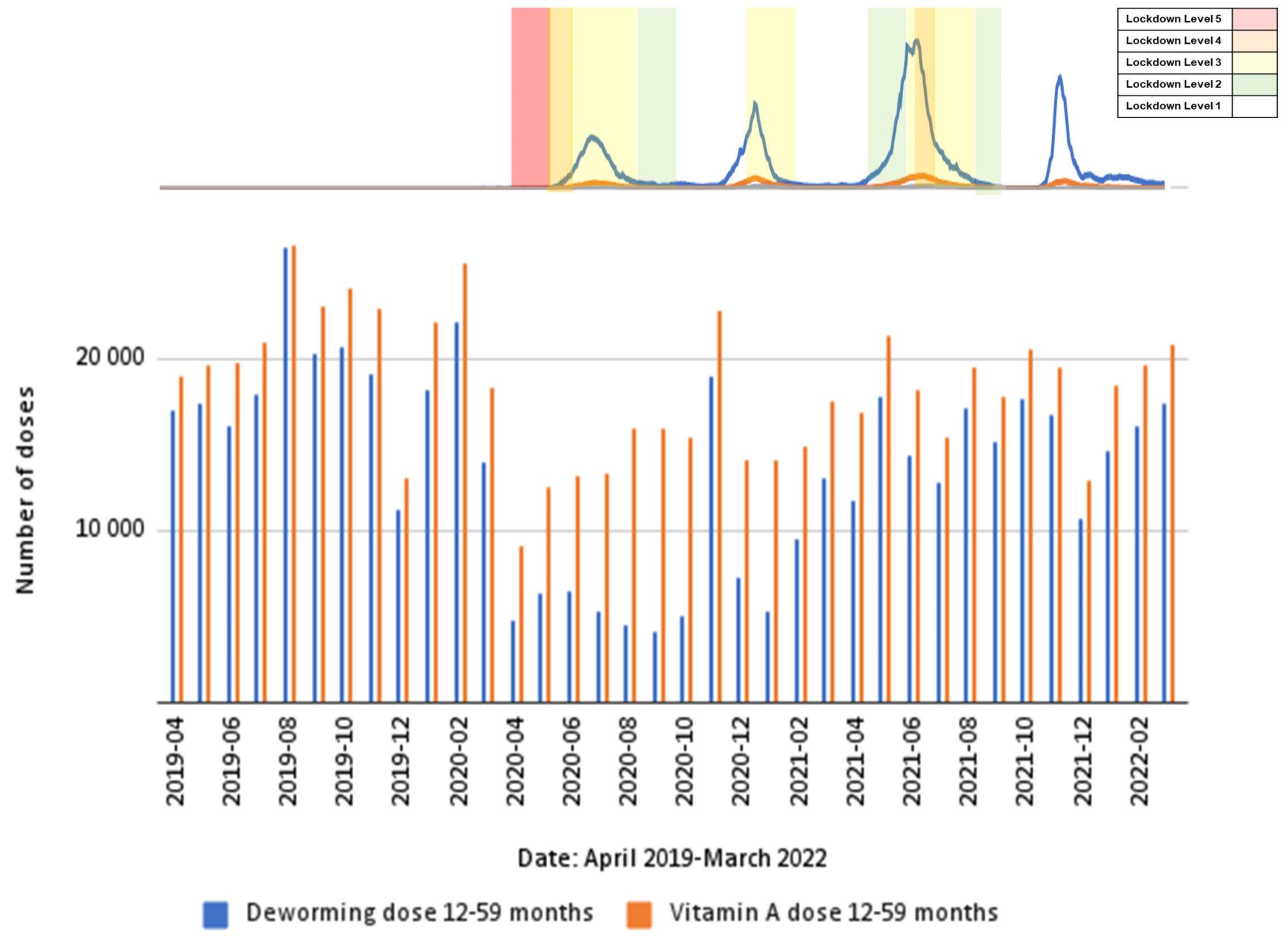
Deworming and Vitamin A supplementation
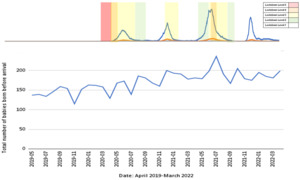
Administration of both Vitamin A supplementation and deworming medication is mainly conducted at PHC facilities and at community level (including administration by community health workers). Both of these preventive health services were reduced by more than 50% during the level-5 lockdown compared with the pre-COVID-19 period, with subsequent improvement in the former as the lockdown restrictions eased (Vitamin A: p=0.002; deworming: p=0.0005; pre-pandemic versus pandemic period) (Figure 12).
Childhood immunisations
The well-established childhood immunisation programme includes multiple vaccinations given at various time points, with the most intensive phase being the first year of life (nine different vaccines, 13 administrations, and seven time points). It is mostly a facility-based health programme, monitored by various data elements and indicators on the DHIS. The measles vaccination (given at six and 12 months of age) is an important coverage marker due to the risk of outbreaks of this highly contagious infection when herd immunity decreases. Another important coverage marker is the data element ‘immunised fully under 1 year’, defined as a child who has completed his/her primary course of immunisation before the age of one year.
Figure 13 shows the effect of the pandemic on these indicators. The figure also shows a yearly decline during each December, including the pre-pandemic period, corresponding to the holiday period. However, the start of lockdown in April 2020 shows a similar sharp decline, with the measles first dose coverage plummeting to 62.8%, but there is evidence of catch-up as the yearly averages moved from 86.2% (pre-pandemic), to 87.8% (2020-2021), and to 90.6% (2021-2022). Additionally, there is evidence of increases in the fully immunised group at the end of the study period (average of 92.7% from January to March 2022) (p<0.001 for 2020-2021 versus 2021-2022)
School health: Screening of learners
The Integrated School Health Programme (ISHP) provides a comprehensive screening programme (including vision, speech and hearing, anthropometry, locomotor system, oral health, communicable and non-communicable diseases, mental health and psychosocial risk) for all Grades 1 and 8 and other at-risk learners, undertaken by 23 dedicated teams in Tshwane District during school terms. The screenings are done on site, and screening periods are limited to public school terms. Figure 14 shows the severe ISHP disruption for multiple months in 2020 and 2021 due to COVID-19-related school closures from 18/03/2020, with partial school re-openings from 08/06/2020 and renewed closures from 27/07/2020 to 03/08/2020, with phased reopening thereafter.
Human papillomavirus (HPV) immunisation
The HPV immunisation campaign is a national school-based vaccination campaign implemented through the ISHP in all public schools. Female learners in grades 4 or 5, aged 9 years and older, are given two doses at six-month intervals, in two campaigns (February/March and August/September). Table 1 shows the relevant data for Tshwane District for 2019-2022.
Review of overall trends for the selected indicators show that most routine MNCWH services were disrupted during the COVID-19 pandemic period, with more severe impacts on preventive services at PHC and community level than on facility-based clinical services (Table 2). The most significant decrease was experienced during the first pandemic year, most notably during the first strict lockdown period, with partial or complete recovery in the second pandemic year.
Discussion
South Africa has seen improved maternal and child health outcomes in the past decade, linked to improved effectiveness and access to large-scale health programmes, mostly anchored in PHC services at district level.5 These routine services are accessible to all citizens and mostly free of charge through the public health system. The data presented in this chapter largely exclude curative hospital-based services and services rendered within the private sector.
The COVID-19 pandemic was a major disruptive force, not only due to risk of morbidity and mortality because of infection with this novel pathogen, but also because of the lockdown regulations designed to curb its spread.6 During the initial strict lockdown period, movement of the entire population was severely restricted outside of their homes.7 Although PHC facilities in Tshwane District remained open and mostly functional, apart from short-term closures for COVID-19 prevention activities, uptake of many MNCWH services showed a sharp decline during the initial strict level-5 lockdown, despite very few COVID-19 cases at that stage. Preventive health services were most severely affected, particularly services rendered at community level and at schools/crèches. This decreased utilisation at the onset of the pandemic, with subsequent second-year recovery, is consistent with findings of other African and Indian studies.8–10 Contributing factors included movement restrictions, reduced access to transportation, pandemic-related economic challenges, reduced health-system capacity, and delayed care-seeking behaviours due to fear of infection and misconceptions about transmission. Clients were more likely to avoid or delay routine or preventive services than to delay acute and emergency medical care. This was in line with reports by Czeisler et al.11 that one-third of adult American respondents delayed or avoided routine medical care during June 2020.
Utilisation of family-planning services decreased markedly, as indicated by the significant decrease in CYPR. However, whereas this decrease reversed in the second pandemic year in the rest of the Gauteng12 it did not do so in Tshwane District, where it decreased further. The national shortage of injectable medroxyprogesterone prior to and during the pandemic period also affected Tshwane District and may have contributed to some extent to the low CYPR. The cervical cancer screening programme was also significantly impacted, especially during the initial strict lockdown period, possibly because it was not deemed to be immediately life-threatening if temporarily postponed. The discrepancy in cervical cancer screening data from the DHIS and the NHLS, particularly during level-5 lockdown, can likely be attributed to data-quality issues, including incomplete facility-level capturing, similar to reports from other sites during the pandemic.2,13 The decreased cervical cancer screening led to reduction in early detection of high-grade precancerous lesions, raising concerns about long-term impacts of the missed screening opportunities during the pandemic.
Additionally, the HPV immunisation campaign was significantly affected by COVID-19-related school closures, with the pandemic onset coinciding with a planned change-over in age group of vaccine-eligible girls in 2020, leading to very low HPV numbers in the first pandemic year. On resumption in 2021, the service showed the ability to adapt, despite the erratic school calendar caused by the pandemic’s lockdown restrictions, but long-term concerns remain regarding missed HPV vaccinations during this period. Adolescents engaging in risky sexual behaviour are at high risk for HPV infection and more than 90% of HPV-associated cancers are preventable through vaccination.14
The inability of community health workers to conduct their usual home visits during the lockdown period to administer routine health interventions is illustrated by significant reductions in Vitamin A and deworming administration. Health screening of learners at schools was also severely disrupted by COVID-19 restrictions, with schools closed for most of 2020, and partial or rotational return of learners still prevalent in 2021. Children who missed preventive healthcare opportunities are at risk of never catching up on these, except if catch-up activities are subsequently prioritised within the health system.
One well-established preventive health programme that showed resilience in Tshwane District was the childhood immunisation programme, despite the programme being known to easily take strain during crisis situations.15 Data in this study showed immediate large decreases at the start of the pandemic, but then marked increases in both measles and fully immunised (under-1-year) indicators during the second pandemic year, to levels higher than pre-pandemic coverage. Importantly though, despite such successes, a significant number of children who missed vaccinations during the acute crisis period may still not have had catch-up doses, leading to population-level reductions in herd immunity and risks of vaccine-preventable disease outbreaks, as illustrated in the current country-wide measles outbreak.16
In September 2019, the high pre-existing level of gender-based violence was declared a national crisis by the South African government. Global research showed an increase in domestic violence during the COVID-19 lockdown period, with increased numbers of gender-based violence cases reported in the first seven days of strict level-5 lockdown in South Africa.17 However, limited local research has been done on the impact of lockdown restrictions on women’s and children’s experiences of domestic violence, including intimate partner violence and child abuse. Research done by Mahlangu et al.18 in Gauteng, South Africa, reported that women experienced increased levels of emotional abuse and reported higher levels of paternal physical abuse towards their children, but notably few women reported experiencing physical violence at home. In the present study, the number of clients reporting sexual abuse at the forensic clinical services decreased markedly during the strict lockdown periods. Possible explanations include movement restrictions, night-time curfews, limited social events, and the lockdown-related alcohol ban, potentially decreasing the risk of sexual assault. But the restrictions could also have prevented clients from accessing services and reporting abuse, with children and victims of domestic violence being particularly vulnerable groups.
The significantly improved TOP access in Tshwane District over the study period shows that health-service disruption can be mitigated and even counteracted by planned resource allocation, even when faced with a crisis of the magnitude of the COVID-19 pandemic, with its associated lockdown measures. Gauteng was the only South African province that did not report a decrease in the number of TOPs during the pandemic.19
The increased number of teenage deliveries and the number of babies born outside of health facilities recorded during the study period in Tshwane District is of concern, with trends continuing into the second year. Several factors, including transport issues and precipitous labour, could have led to women giving birth before arrival at a health facility, but preference for home deliveries reportedly also increased, particularly among refugee women.20,21 Nationally, the teenage in-facility deliveries rate increased during the pandemic, although overall teenage pregnancy rates are difficult to calculate because of inaccurate reporting of pregnancies ending in miscarriages or terminations. Pandemic-related school closures and disruption of access to family-planning services, together with previously identified predictors of teenage pregnancies such as lack of parental support and economic challenges, possibly put teenagers in Tshwane District at compounded risk of unplanned pregnancies.19
In the present study, MNCWH services that were linked to clinical care provision were less disrupted than preventive services. Despite early concerns regarding the risk of contracting COVID-19 during visits to health facilities, utilisation of antenatal services in Tshwane District was generally well maintained throughout the pandemic. This also extended to in-facility components of large-scale health programmes, such as infant HIV PCR testing. Research from Johannesburg, South Africa, on infant HIV diagnosis during the pandemic utilising NHLS data similarly found minimal disruption to HIV testing for children under two years of age.22
Stillbirth numbers increased significantly during the first pandemic year, in line with international research done by Khalil and colleagues.23 However, unlike many other indicators studied in this research, the noticeable spikes coincided with the first and second COVID-19 waves, rather than with lockdown periods. It is unclear whether this was due to maternal SARS-CoV-2 infection, or the additional strain on healthcare resources during times of increased infections and admissions.24
The strengths of this study include the use of district-wide data from several sources from one of the country’s large health districts, with many of the researchers, as staff members of the Tshwane District Health Services, having intimate knowledge of the health-service provision in the district. Limitations include the use of routine data sets with all the inherent difficulties in terms of completeness and correctness, particularly during a time of crisis impacting health workers and administrative staff, although data cleaning was done as far as possible. Local geographical variations may have been obscured by the presented aggregate district-level data. Furthermore, there was a lack of private-sector data with regard to routine data sets, excluding the COVID-19 surveillance data. Quantitative data alone are not sufficient to fully unpack the reasons for particular health-seeking behaviour. In addition, the COVID-19 pandemic and the associated lockdown measures led to changes in both internal and external migration patterns influencing health-service needs in terms of access in specific geographical areas, which was not measurable as part of this research.
Conclusions and Recommendations
The COVID-19 pandemic has been a major challenge to health services globally. The research presented in this chapter indicates its impact on the ability of women and children to access various routine healthcare services in a large peri-urban district in South Africa. Future-proofing the health system for major disruptive events, such as pandemics, needs to include planning of service delivery and client access to service-delivery points at all levels of care, including at community level. While curative services may need to be prioritised in the acute phase, it is crucial that the likely duration of an emergency situation be regularly reassessed, with delivery of preventive services also prioritised, despite the emergency situation. Measures that need to be strengthened include use of innovative digital health solutions to assist with health education, and where possible, appointment reminders and use of telemedicine for routine consultations.
The Tshwane Maternal-Child COVID-19 Study was established to study the burden and impact of the COVID-19 pandemic on maternal and child health in the Tshwane District, South Africa. It was registered under the reference number 822/2020 with the Ethics Committee of the Faculty of Health Sciences, University of Pretoria, South Africa.





_first_visits_done_in_tshwane_district_from_april_2.png)
_in_tshwane_dis.png)







_first_visits_done_in_tshwane_district_from_april_2.png)

_in_tshwane_dis.png)